This case study documents the work of Gaylord Long-Term Acute Care Hospital’s (LTACH) respiratory care department to improve patient outcomes for its long-term ventilator/tracheostomy patients by implementing heated high-flow humidification.
Gaylord Specialty Healthcare is a rehabilitation-focused, nonprofit health system in Connecticut that provides inpatient and outpatient care for people at every point in their journey from illness and injury to maximum recovery. The system is anchored by Gaylord Hospital, a Long-Term Acute Care Hospital, and includes Gaylord Outpatient and Gaylord Physical Therapy for patients who require diagnosis and treatment on an outpatient basis. Together, these entities deliver a complete continuum of rehab care driven by technology, research, clinical experience, and human compassion.
In 2012, Gaylord Hospital tasked the Respiratory Department with improving their outcomes. I had recently joined the department as supervisor, and together with the department’s new director, we were determined to make positive changes, raise the bar, and strategize ways to improve our results.
We reviewed the percentage of ventilator patients who successfully weaned from the ventilator and the number of tracheostomy patients who were successfully decannulated. We noted that the tracheostomy population, whether on the ventilator or off, struggled with thick secretions, mucous plugs and difficulty maintaining a patent airway. This translated to longer days on the ventilator. Gaylord at this time had an average of 20-22 days to wean off the ventilator. Our wean rate was consistently in the low 60’s and with the national average reported as 50-60% by many sources, we wanted to do better. The hospital also had a ventilator-associated pneumonia (VAP) rate that the department wanted to decrease.
We were using pass over humidification on our ventilators and cool mist for our trach patients. Heated high-flow humidification via high-flow devices had been used at many acute care facilities with the nasal cannula interface to provide adequate humidification and flow to patients. Our director had previous experience with the benefits of heated high-flow humidification, therefore we decided that in addition to adding active heated humidification on our ventilators, heated high-flow humidification would be the standard of care for all ventilator weaning and tracheostomy patients. This use was not the standard of care in the LTACH environment. However the ventilator patients that come to the LTACH level of care typically are on the ventilator for weeks or even months prior to the transfer. Many acute care hospitals utilize active humidification on these longer term ventilator patients to keep their secretions mobilized. We sought to continue the adequate humidification when the patients were off the ventilator.
Implementing this change in practice was a significant undertaking at our facility. The staff was initially hesitant due to the standard of practice at most institutions being cool mist humidification. Early on in this process, staff began to comment on the increased suction needs of the patients once heated high-flow was started, but after they began to realize it was not producing more secretions, but rather mobilizing retained secretions, the staff started to understand the benefits. We provided extensive staff education to ensure buy-in and once some staff began to champion the change, others followed suit. We then removed all cool mist from the facility. We also changed our vent weaning protocol to reflect that heated high-flow would be used when patients are removed from the ventilator during weaning.
When Gaylord began this process change in 2012, most LTACHs provided humidification for tracheostomy patients in the form of a cool mist. This system delivered a cold mist that did not achieve deposition beyond the upper portion of the trachea. The system was cost-effective, costing approximately $10.00 or less per patient. Some facilities also used HME (heat moisture exchanger) devices, which are also cost-effective with an average cost of $2.50 each. We decided to purchase a heated high-flow humidification system, which was costly in comparison, averaging approximately $3,000 each unit at this time. Our goals were to decrease ventilator days, ventilator-associated pneumonias and issues with airway clearance and mucus plugging by using heated high-flow humidification. This would translate to cost savings and improve care for our patient population. Fortunately we had a leadership team in place that was willing to support this practice change and trust in our plan.
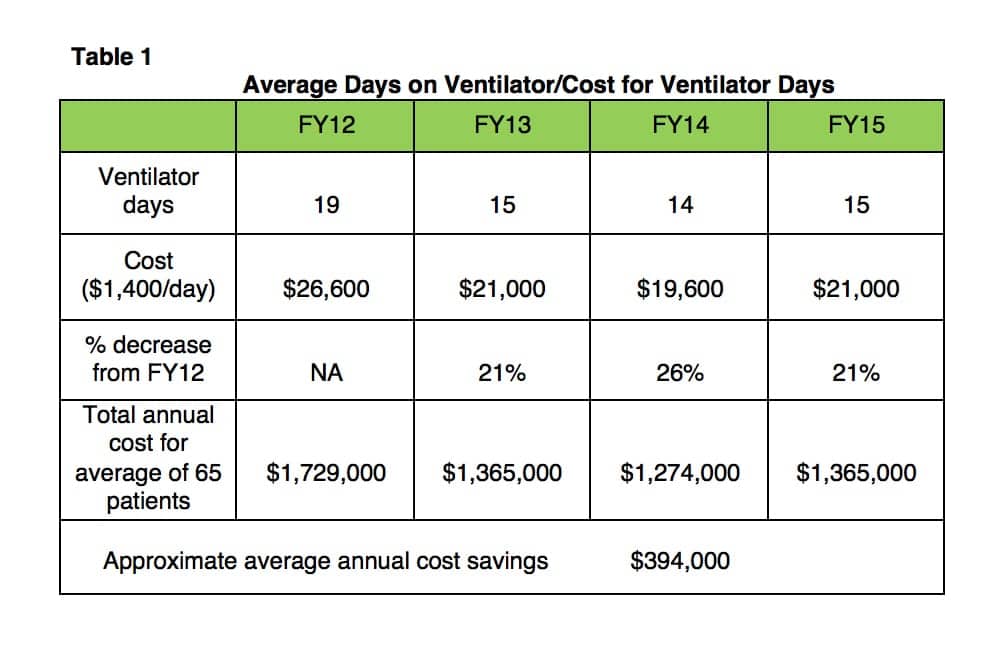
The success of this initiative was realized in our outcomes and metrics in the following fiscal years. The measurement indicators we evaluated to gage success were ventilator days for successfully weaned patients, the ventilator-associated pneumonia rate and the number of tracheostomy decannulations. We included data from FY12 as our baseline and FY13-FY15 for comparison. In FY12 the average days on the ventilator for weaned patients was 19. After heated high-flow humidification became the standard of care, the average days decreased to 15 in FY13, 14 in FY14 and 15 in FY15. Ventilator-associated pneumonias (VAPS in 2012) were at a rate of 4.1 (per 1,000 vent days). In 2013 this measurement was renamed as Ventilator-Associated Events, per the Centers of Disease Control (CDC) and National Healthcare Safety Network (NHSN) guidelines. In FY13 our rate was 2.0, the FY14 rate was 1.0 and the FY15 rate was 0.
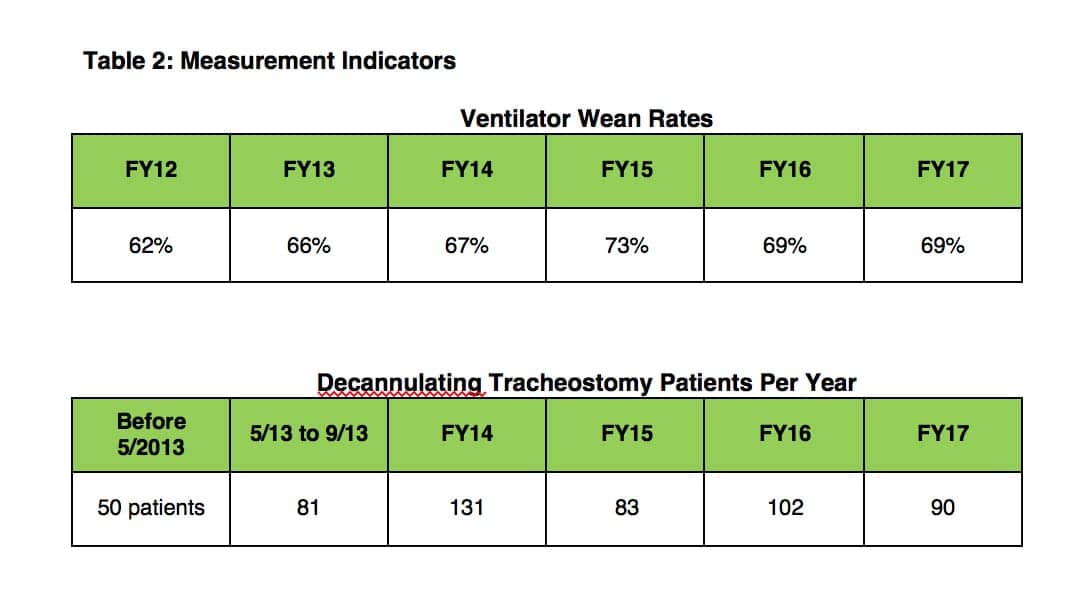
In addition to the changes we had anticipated, we began to take notice of our decannulation numbers since we changed our process. Previously we were decannulating approximately 50 tracheostomy patients per year. As we noticed our tracheostomy decannulations increasing, we began to track this metric closer starting in May 2013. From May 1, 2013 to September 30, 2013 we decannulated 81 patients. In FY14 a total of 131 patients were decannulated. In FY15 we decannulated 83 patients. Successful decannulation improves patients’ quality of life and it positively impacts their discharge disposition. It is often difficult for a patient to discharge to home or the skilled nursing facility of their choice with a tracheostomy tube in place. Decannulating patients improves their options for the discharge destination of their choice.
Besides the impact on outcomes we expected to see, we also noted we were performing significantly fewer bedside bronchoscopies for mucous plugging and secretion-related issues. We had previously averaged one to two per month and now we were averaging one to two every six months. Since we were providing adequate humidification, we were not experiencing the mucous plugs and plugged tracheostomy tubes we had seen in the past. Fewer issues related to mucous plugging also translated to quicker ventilator weans for our patients with fewer airway clearance complications. This also contributed to our ability to increase our tracheostomy decannulations.
One of the challenges we foresaw when making the transition to heated high-flow humidification, was justifying the cost of the equipment to the organization’s leadership. We used our outcome improvements to do so. The biggest financial impact realized was seen in the decrease of ventilator days. A ventilator day at our facility costs an average of $1,400.00. Ventilator days were decreased by an average of 4.33 days. This translated to a cost savings of $6,062.00 per patient. From 2013-2015 we had an average of 65 ventilator wean patients per year. Decreasing the days on the ventilator for this population by 4.33 days translated to a savings of $394,000 per year.
The decrease of ventilator-associated pneumonia cases also contributed to a cost savings. A ventilator-associated pneumonia is estimated to cost $40,000 per hospital admission.1 As previously mentioned, our VAP rate decreased steadily after we changed our practice, from 4.1 in 2012 down to 0 in FY15. The estimated cost savings based on the decreased VAP rate for FY13 was $80,000. FY14 estimated was $120,000 and FY15 estimated was $160,000.
An additional benefit we noted when using heated high-flow humidification, was the ability to adjust flow which increased comfort for patients while breathing off the ventilator. We were able to meet the patients’ needs and this eliminated the feeling of air hunger and therefore decreased work of breathing. This translated to better wean rates for our ventilator population. Our ventilator wean rate was 62% in FY12. After these changes we saw steady improvement with our rates at 66% in FY13 and 67% in FY14. In FY15 the rate was at 73%.
The next logical step for our facility was to look at our outcomes and see if they remained consistent over time, especially as we noticed our ventilator wean referrals changing. In FY16 we averaged 17.9 days to wean, a wean rate of 69% and 102 decannulations. In FY17 we averaged 14 days to wean, a wean rate of 69% and 90 decannulations. This evidence showed us that our data was remaining consistent over time, even though our patient population was changing. We started to note it was becoming more challenging to get insurance approval for a patient to come to our facility for ventilator weaning. The patients we were getting had increased comorbidities and had been at the acute care for significant time periods before coming to us. This translated to a more deconditioned patient, which could negatively impact weaning time.
Our hospital learned several significant lessons from this process change to heated high-flow humidification. We realized cost savings in our outcomes measurements as we saw improvement in several key metrics. We also saw positive results in terms of our increased tracheostomy decannulations. Increasing decannulations allowed us to discharge the tracheostomy patients to the destination of their choice more often. This improved patient satisfaction and contributed to increased quality of life, as many of our patients and families told us what a huge value it was to have the ability to discharge to their preferred location.
We also recognized that the use of heated high-flow humidification on ventilator weaning patients not only provided oxygenation and better humidification, but also improved their weaning tolerance through our ability to increase flow. The impact of this was seen in our increased ventilator wean rates. After evaluating our outcomes through FY15, we shared our results with other LTACHs in the hope of changing practice for ventilator weaning and tracheostomy patient care. We hope to influence best practices in the LTACH environment to improve patient outcomes and quality of life.
Lorraine Cullen MS, RRT, RRT-ACCS has been in the field for 25 years. She started her career as an AS, RRT and earned her BA degree in 2001. In 2015 she completed her MS degree in Healthcare Leadership. She has worked in both the acute care and LTACH environment, starting her career in acute care and working at two LTACHs throughout the last 15 years. Since 2012 she has worked at Gaylord Hospital, an LTACH in Connecticut, first as the Supervisor and currently as the director of Respiratory Care.
Gaylord Specialty Healthcare is a rehabilitation-focused, nonprofit health system that provides inpatient and outpatient care for people at every point in their journey from illness and injury to maximum recovery. Gaylord Specialty Healthcare is widely recognized for its leadership in treating spinal cord and brain injuries and is also known for treating pulmonary, cardiac, amputee and stroke patients as well as sports-related injuries. It is the only rehabilitation system in CT accredited by CARF (Commission on Accreditation of Rehabilitation Facilities) for both inpatient and outpatient programs. Gaylord Specialty Healthcare is anchored by Gaylord Hospital, a Long-Term Acute Care Hospital, and includes Gaylord Outpatient and Gaylord Physical Therapy for patients who require diagnosis and treatment on an outpatient basis. Together, these entities deliver a complete continuum of rehab care driven by technology, research, clinical experience, and human compassion. Headquartered in Wallingford, Conn since it was founded in 1902, Gaylord today serves a mix of local, regional, national, and international patients.
References
- Kollef, MH, Hamilton, CW, Ernst, FR. Economic impact of ventilator-associated pneumonia in a large matched cohort. Infection Control Hospital Epidemiology. 2017;33(3):250-256.
- Guterl, GO. Cost Implications of VAP: An equation developed by Johns Hopkins helps administrators quantify potential savings by reducing hospital-acquired infections. Advance for Respiratory Care and Sleep Medicine. 2013. http://respiratory-care-sleep-medicine.advanceweb.com/Features/Articles/Cost-Implications-of-VAP.aspx.











Do you change out ventilator circuits at all? How often do you change your in-line suction?
We change our circuits every 28 days or when visibly soiled. We change our inline suction caths every 72 hours.