In January 2013, the Centers for Disease Control and Prevention (CDC) implemented a new algorithm for the identification of ventilator-associated events (VAEs). Under these new standards, respiratory therapy professionals will now identify and report ventilator-associated pneumonia (VAP), along with other ventilator conditions, to the CDC’s National Healthcare Safety Network (NHSN) based on more uniform and objective diagnostic criteria.
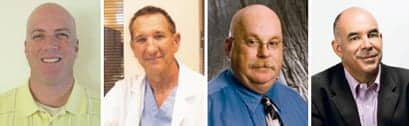
To help understand the impact of these changes on respiratory care departments, on management of ventilated patients, and on data collection and reporting, RT Magazine convened the following panel of experts:
Michael V. Frey, BS, RRT-NPS, Clinical Consultant, Respiratory Technologies – Ventilation and Alternate Care, CareFusion;
Mark Grzeskowiak, RCP, RRT, FAARC, Manager of Education & Quality, Respiratory Care Services, Long Beach Memorial Medical Center, Long Beach, Calif;
Michael J. Hewitt, RRT-NPS, FAARC, FCCM, Chair-elect, Respiratory Section, Society of Critical Care Medicine;
Carlos M. Nunez, MD, Chief Medical Officer and Senior Vice President, Medical Affairs, CareFusion.
RT: Prior to the changes in VAE standards, did your department participate in VAP reporting to the CDC’s National Healthcare Safety Network?
Mark Grzeskowiak: Yes, we did. We felt it was a good way to compare ourselves to a standard of patient care. We also thought that this data could be reviewed by the general public or other groups that report on health care quality issues to the general public.
Michael Hewitt: Yes, we did. It is important to be able to benchmark with other similar facilities and practices. Having said that, prior data collection may not have been as robust and objective as would be required for accurate analysis and comparison.
RT: If you did previously report, will you continue to participate under the new standards? If you did not previously report, will you begin to participate?
Grzeskowiak: We will not. It is a very labor-intensive process. We will continue to monitor internally. I think it’s entirely possible that other respiratory care departments will also choose not to participate. Our hospital has five people who conduct surveillance. They tell me they stay pretty busy monitoring for the usual hospital-acquired infections (bloodstream, catheter-associated urinary tract infections, and surgical site infections). Having to check the ventilator records to review a patient’s PEEP/FiO2 requirements is simply more work than they can do. I can imagine that it is even more challenging at smaller hospitals where people typically wear more than one hat. Another point to consider is that there is no financial penalty for not participating.
RT: How do the new standards increase the ability for automation? Do the VAE/VAP definition and algorithms make it more feasible to collect and report data in an automated fashion?
Michael Frey: I do believe the new VAE algorithms allow the practitioner to report in a more objective measurement. It removes the subjective guesswork from various conditions, for example, x-ray readings. This would allow for a more consistent approach to VAE and allow us to focus scarce resources to true VAE needs. The cost of health care is a staggering amount, and reduction must happen, even if it’s by something as simple as hand washing, for example, which has been proven to be an effective and realistic way to reduce hospital acquired infections. The new VAE algorithms will allow us to be able to realistically monitor and prevent VAE in a measurable way.
Hewitt: I think that this is yet to be seen and will be heavily dependent on the amount of time and resources each facility will devote to gathering of the data. The new definition and algorithms will require more dedicated and invested resources.
Carlos Nunez: Because the new standards are based on objective data, much of the data should be able to be captured in a modern EHR. This allows for a greater opportunity to automate collection—with the right tools—and reporting to the NHSN within the CDC.
For example, two of the most important pieces of data for the algorithm are patient levels of PEEP and FiO2. Both of these measurements can help determine if the patient is progressing toward breathing on his or her own, and they should be collected and reported. They are not subjective determinations made by a clinician, but are objective data points coming right from the ventilator, making automated collection easier. However, it needs to be stressed that in order to get these data into an EHR, the ventilator needs to have the ability to communicate to the hospital information system.
RT: Do you believe the new VAE standards make sense? Will the changes improve the day-to-day care and treatment of patients and the ability of hospitals/practitioners to manage the use of mechanical ventilation?
Frey: I do believe the new VAE standards make sense. They are based on readily available objective data sets that can contribute to better patient care. They also eliminate the subjective data that often could lead practitioners down a wrong road of patient care. They allow for the practitioner to coordinate care within a guideline set that allows various departments to work together. The example could be the FiO2 data set. If the FiO2 data set increases, thus worsening oxygenation status, this will throw up a red flag. Nursing, as well as respiratory caregivers, can be involved and coordinate to help each other recognize potentially deteriorating patient conditions earlier in the process.
Grzeskowiak: In my hospital, opinions on this issue vary greatly. Some physicians want to focus on the administrative aspects. They think there were obvious problems with the previous system but the new system has gone too far. Others think that there may actually be fewer cases of VAP because the radiology component has been eliminated. We have had a few cases where infiltrates could be classified as “persistent” and a physician wrote “possible VAP.” However, the patient’s requirement for oxygen and PEEP did not change so a diagnosis for ventilator-associated complications (VAC) and VAP could not be made. It is my opinion that if we expect this system to have an impact on outcomes, this can only happen in an environment where patient care is a collaborative effort. There are a lot of factors that could contribute to VAE and ventilator management is only one of them. Health care providers will need to see the big picture if they expect to see reduction in VAE. If protocols and daily bedside rounding are used and the lines of communication between all caregivers are open, then there is a chance.
Nunez: I believe the new VAE standards are an improvement from the old standards for a couple of reasons. First, the previous VAP reporting standards were bundled with all pneumonia reporting, regardless of whether the patient was ventilated or not. The new reporting standard and new algorithm are looking at specific events for patients who are on a ventilator. Second, the new standards are looking at objective data. The standards dictate the collection of specific objective data targeted to ventilated patients, and they are much less open to the subjective assessment that increases variability. For example, the old standards included an assessment of a chest x-ray, which is very subjective and can vary widely, particularly across different hospitals. These changes have the potential to improve care if the hospital collects the data and maintains the data in a way that is conducive to performing analytics. Raw data just shows which patients are having an event. It is the hospital’s responsibility to look at all the raw data to see what those patients have in common. What treatments and protocols were they receiving? They should also look at the data to determine the similarities in care for those patients who did not have an event. Why did different patients have different outcomes? What trends can be found? Identifying patients with an event is only the first step. With analytical tools, we can learn from the data and change or reinforce best practices.
RT: Have the new standards had any impact on how respiratory care departments are working with other departments?
Grzeskowiak: Yes, our department reviews the PEEP/FiO2 requirements for all ventilator patients. These values are entered onto a spreadsheet and tracked as long as the patient is on the ventilator. If the patient’s condition worsens and they meet the criteria for VAC, this is forwarded to the hospital’s epidemiology department.
RT: What product features on existing ventilation technology are most helpful in identifying and preventing VAE?
Nunez: The most important feature for mechanical ventilators is the ability to communicate with a hospital’s information system, so it can collect and make available raw data for reporting and analytics. The second most important feature is having the analytical tools to take the data collected and easily and efficiently provide actionable intelligence and track trends in both those who do have events and those who do not. Collecting and understanding the data from a hospital’s ventilated patients is the single most effective tool to identifying and preventing VAEs.
RT: Given the new VAE definitions and algorithms, how are the new reporting standards affecting current ventilation-related products and their instructions for use?
Nunez: I don’t believe the new definitions affect instructions for use at all. They do not change the proper use of a ventilator. Instead, they put more emphasis on the connection with a hospital’s IT infrastructure and the tools and software that come with the ventilators to collect, analyze, and report the data. Today’s ventilators should provide reports and analytics internally to the hospital for comparative analysis and for reporting to external parties like the NHSN. So it’s not the ventilators themselves or the instructions for use that are changing, but a change to the larger ventilation “system” of which they are a part.
RT: How will ventilation technology respond to the new standards, moving forward?
Frey: Mechanical ventilation standards are going to have to switch from a standalone ventilator to an increasingly connected information portal. The ability to monitor and actively evaluate the patient’s condition in real time would be an added safety net and, in some cases, preventative to VAE. The health care practitioner’s ability to have access to and receive pertinent data in real time would be invaluable and in effect could help reduce the costs of medicine. If VAE could be treated in the early stages, thus reducing the need for prolonged mechanical ventilation, the cost savings could be staggering. The average cost for a mechanically ventilated patient is approximately $2,300 per day. After day four, the average cost goes to nearly $4,000 per day. So it is imperative in today’s health care marketplace that we wean patients off mechanical ventilators as quickly and safely as possible.
Nunez: I believe we are going to see more ventilator manufacturers adopt a strategy that the “box” (the mechanical ventilator) is not always the most important product in the ventilation “system.” Hospitals need to have a ventilation system strategy, which includes the ventilators, connectivity to the health IT infrastructure, data collection abilities, data analytics, and reporting tools. It’s not about just connecting patients to ventilators, but gaining insight into the care provided, the complications that may arise, patient outcomes, and a better understanding of managing patients through those outcomes. That can’t be done with a ventilator alone. RT
Mike Fratantoro is managing editor for RT. For further information, contact [email protected].