RT Magazine examines the ways that the COVID-19 pandemic has affected pulmonary function testing labs and some of the precautions they are taking when conducting PFT for non-COVID-19 lung diseases.
The COVID-19 pandemic has infiltrated every aspect of healthcare. While emergency and critical care units treating coronavirus-positive patients continue to be most affected, the virus has also taxed other hospital units and many non-COVID-19 patients, as elective and non-emergency procedures have been delayed or postponed. One of these affected units is the pulmonary function testing lab.
In early March, the American Thoracic Society’s Proficiency Standards for PFT Committee said the risks of coronavirus transmission in PFT labs may be “significant” and recommended PFT be limited to essential tests. “Decisions regarding the conduct of pulmonary function tests need to balance the potential risks against the need for assessment of lung function to make treatment decisions,” the committee wrote. Likewise, the American College of Occupational & Environmental Medicine recommended suspension of all non-emergency PFT. “Spirometry tests require performance of a forced expiratory maneuver which could spread droplets in the air if an infected person is tested, even if asymptomatic,” the ACOEM said in a statement.
In order to find out how PFT labs are functioning during the pandemic, RT spoke with the following pulmonary function testing experts about the state of their labs:
- Cheryl A. Hoerr, RRT, MBA, Director of Respiratory and Sleep Services, Phelps Health (Rolla, Mo) and Vice President, Internal Affairs, AARC Board of Directors;
- David A. Kaminsky, MD, Medical Director, Pulmonary Function Laboratory and Pulmonary and Critical Care Physician, University of Vermont Medical Group;
- Dave Shuldes, RRT, Respiratory Therapy Manager, St Luke’s Health System (Boise, Id);
- Ralph W Stumbo Jr, RRT, CPFT, Owner and president, Apex Pulmonary Solutions LLC, RT/PFT, Group Health Cooperative (Tacoma, Wa), and AARC Diagnostics Section Chair.
1. How has the COVID-19 epidemic affected your PFT lab? Has it affected the number of PFT procedures your lab has conducted?
HOERR: We have two PFT testing locations; one located within the Respiratory Therapy department of the hospital and the other located in a physician clinic across town. Out of an abundance of caution we elected to completely close both of our PFT testing areas beginning on March 23. Fortunately, due to the very low incidence of COVID-19 in our county, our organization is planning to reopen our diagnostic testing areas on May 4.
KAMINSKY: During the peak of the pandemic in our region the lab was reduced from 5-6 staff to two. We maintained staffing in case there was the need for an essential PFT, but we ended up testing only 3-4 patients per week. We are now reopening as of this week with the requirement for all patients to have COVID testing prior to testing starting next week.
SHULDES: We have been conducting emergency inpatient PFTs only—required for surgery and BMT procedures. All outpatient PFT’s have been suspended since March.
STUMBO: We are only seeing urgent patients from specific diagnoses after they have been screened by our pulmonologist.
2. Has the virus affected your lab’s open hours or staffing numbers?
HOERR: PFT testing within the hospital was completely closed throughout. However, we did test several patients at our clinic site due to the emergent nature of their needs (eg pre-op, complications of chemo, etc).
KAMINSKY: Same hours, markedly reduced staffing. Our staff also assist with all bronchoscopies, so we had two technologists working a day rather than the usual 5-6.
SHULDES: Yes, we have floated our staff to RT, or kept them home on payroll protection.
STUMBO: No, PFT lab hours have not changed.
3. Have any staff been reassigned to support other clinical areas, for instance COVID-19 patient care?
HOERR: The hospital PFT staff were absorbed into the Respiratory Therapy department staffing. The therapist who does PFTs at our off-site clinic was repurposed to do various other duties within the clinic: patient screening at the front door of the clinic, helping with blood draws in the clinic lab, and assisting physicians with patient assessment and treatment.
Our organization did stand up our labor pool and if other work had not been available then the PFT staff would have been able to make up their hours with reassignments throughout the organization—eg patient screening at entry points, screening tent, storeroom duties, etc. (That’s what my Sleep Center staff has done for the past weeks.)
KAMINSKY: Yes, some staff voluntarily were reassigned to work on the floors and in the ICUs.
SHULDES: Our PFT techs are all RRT’s and have been re-assigned to regular RT patient care.
STUMBO: Some staff have been reassigned to others area to support other activities. We are not attached to a hospital so they were not typical RT duties but work that needed to be performed.
4. How is your lab/facility using telehealth to conduct or manage PFT?
HOERR: No telehealth is used by PFT services. Most of our providers are using telehealth for patient visits but we have not implemented it for PFTs.
KAMINSKY: We are not using telehealth in the PFT lab. It is only being used in the outpatient clinic and for ICU consultation requested by outlying community hospitals.
SHULDES: None at this time.
STUMBO: We have gone from about 25% telehealth to greater than 80%.
5. What personal protective equipment policies has your lab adopted to keep clinicians and patients safe?
HOERR: Therapists must wear a surgical mask, face shield/goggles, and gloves during testing. We routinely deliver bronchodilators with a MDI and valved-holding chamber, but if we end up nebulizing the bronchodilator then the therapist must wear complete PPE: gown, gloves, face shield/goggles, and an N95 mask. This is a substantial change since we usually don’t wear this equipment during routing PFTs. Additionally, a filtered nebulizer must be used, and once the treatment has started, the therapist will wait outside the room and periodically check in until the treatment is completed.
KAMINSKY: Full PPE with N95 masks for all staff right now until COVID testing starts. Then staff will be required to wear surgical masks.
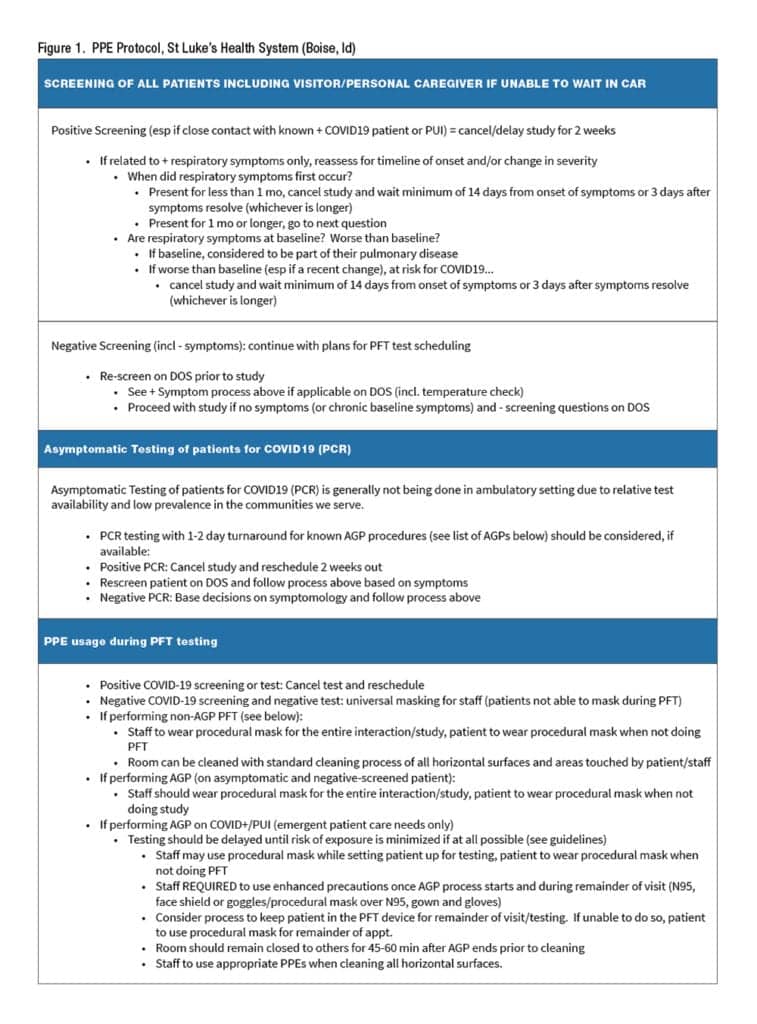
SHULDES: This does not have a brief answer. No PPE was generally used by PFT technicians going into the changes described below unless the patient had a confirmed infectious diagnosis required airborne precautions. See Figure 1.
STUMBO: Patients and staff are checked for symptoms as they enter the building. Those with no fever and no symptoms are given a green dot to wear, others are given an orange dot.
6. Have your equipment sterilization and decontamination procedures changed at all as a result of COVID-19?
HOERR: PFT testing may cause the patient to cough and generate aerosolized particles of virus. We installed a HEPA room air filter to mitigate the risk of aerosolized virus particles. We adjusted the testing schedule to allow for additional time between testing appointments so that the equipment can be disinfected and the room can be wiped down as necessary. Only the patient will be allowed in the PFT lab and family members will wait outside the facility.
KAMINSKY: Yes, we now change the pneumotach in between patients and swap out the breathing circuit for any tests involving DLCO or lung volumes. Otherwise, we are continuing with normal cleaning procedures, but all PFTs right now, when done, are performed in one of our two negative pressure rooms only.
SHULDES: All equipment exterior is wiped down with Sani-cloth after procedure. Per above, PFT tests are not performed on symptomatic or confirmed COVID patients.
STUMBO: Our procedures were set up for worst case scenario so there has been next to no changes needed.
7. What role do bacterial viral filters (BVF) play in infection control and is your lab seeing increased use/demand?
HOERR: We’ve always used a BVF for every test, so that will not change.
KAMINSKY: These are used routinely with no change in practice.
SHULDES: No increase in prior use.
STUMBO: We have always used them as part of our infection control policy so there has been no change.
8. Early diagnosis of chronic lung disease leads to earlier treatment. In general, is the virus delaying diagnoses for lung diseases like asthma and COPD? What impact do you believe it will have on these diseases and what can the industry do to mitigate that impact?
HOERR: Testing might have been delayed but our providers were still seeing patients and treating them appropriately based on patient symptoms and provider assessment, so I don’t think care was delayed even if the diagnosis was preliminary (and pending the PFT).
The most concerning issue I see is that patients are afraid to visit their physicians or come to the lab for testing for fear they will be exposed to COVID-19. This could lead to delayed diagnosis and under-treatment, and could potentially lead to unnecessary hospitalization or needless visits to the ED. Mitigation will be education. When we reopen our lab, we will be providing education and much reassurance to our patients about the current situation and specific actions they can take to stay safe.
KAMINSKY: Undoubtedly this is probably happening, but it is hard to document. We are hoping to get up and running seeing patients again in person in both the outpatient clinic and the PFT lab in order to provide the best possible care.
SHULDES: Yes, the lack of PFT availability since March has very likely resulting in delayed diagnosis. I don’t have data to support that suspicion. Performing PFTs with proper precautions on all but symptomatic or confirmed COVID-19 positive patients is crucially important, which is why we are reopening our PFT lab—we currently have a back-log of 1,300 scheduled patients to work through.
STUMBO: There are going to be significant back-logs of patients needed to get in for initial diagnosis as well as follow-up care. This will delay initial treatments in some cases but I believe most providers would not have an issue with treating people initially based on history and physical and symptoms. They should be able to get some initial treatment and then follow-up with PFTs at a later date.
RT
For more information, contact [email protected].
References
- Arnold RJ, McCormack M and Kaminsky, D. Pulmonary Function Laboratories: Advice Regarding COVID-19. Accessed from www. thoracic.org.
- ACOEM Advises Suspension of Routine Occupational Spirometry Testing During COVID-19 Pandemic. Accessed www.acoem.org.










