Preventing infection, treating reversible symptoms, and educating patients are contributing factors in managing COPD
The term chronic obstructive pulmonary disease (COPD) refers to a spectrum of chronic pulmonary disorders characterized by shortness of breath, coughing, sputum production, airflow limitation, and impaired gas exchange.1 Most patients with COPD have either chronic bronchitis or emphysema. These diseases affect 11 to 30 million people in the United States,1-4 and they represent the fifth leading cause of death.1,3-5
The death rate from COPD has increased 22% during the past decade.1,5 The mortality rate 10 years after diagnosis is more than 50% and this percentage is on the rise.1,5 Cigarette smoking is an important etiologic factor. Prevalence, incidence, and mortality increase with age, and are higher in males than in females.2 Prevalence is especially increasing in females, largely as a result of increased cigarette smoking by women.2
Emphysema is characterized by permanent abnormal airspace enlargement. This enlargement occurs distal to the terminal bronchioles and is associated with destruction of the airspace walls. Chronic bronchitis is characterized by chronic cough, sputum production, and inflammation of the mucosal surfaces of the larger airways.4
In chronic pulmonary disease, the predominant pathology in large airways is mucus-gland hyperplasia. This results in the excess sputum production characteristic of chronic bronchitis.6 Variable degrees of smooth-muscle hyperplasia may also be present. The small airways, however, are the main sites of airway obstruction in COPD. Small airways exhibit characteristic changes, including inflammation, fibrosis, mucus production, and narrowing.
Clinical Manifestations
The preclinical course of patients with COPD is highly variable. Patients with a history of lung disease early in life may exhibit reduced pulmonary function in adulthood. Smoking by patients with a history of childhood lung disease may lead to a progressive decline in lung function. Other patients who smoke probably begin adulthood with normal lung function. Forced expiratory volume in 1 second (FEV1) usually remains within normal limits until middle age, when a rapid decline in pulmonary function ensues.5 Generally, this decline stops in patients who quit smoking. The clinical symptoms of COPD generally will appear in patients who continue to smoke.4
Patients with COPD usually present with shortness of breath, cough, and/or wheezing. Coughing generally indicates excess mucus production. The shortness of breath is a result of increased work of breathing through obstructed airways, and is usually associated, at least initially, with increasing levels of exertion. Over time, the dyspnea worsens to the point of occurring at rest. Wheezing occurs as a result of airway narrowing, mucosal edema, and retained secretions.
Often, patients with chronic pulmonary disease are described as either blue bloaters or pink puffers. Blue bloaters have central cyanosis with secondary polycythemia and edema. Arterial blood gas (ABG) evaluation usually reveals evidence of hypoxemia (Po2: 45 to 55 mm Hg), carbon dioxide retention (Pco2: 50 to 60 mm Hg), and compensated respiratory acidosis (pH: 7.38 to 7.42).4 Pink puffers do not have secondary polycythemia, and edema is not present. They have less hypoxemia (Po2, 60-80 mm Hg) and no carbon dioxide retention (Pco2, 30-40 mm Hg).4 Many patients have features of both conditions.
Spirometry is performed for all patients suspected of having COPD. It is a simple office procedure that is done to assess FEV1 and forced vital capacity (FVC). The FEV1:FVC ratio can then be calculated; it should be determined before and after bronchodilator use. Follow-up spirometry should be repeated after maximal therapy. In chronic pulmonary disease, FEV1 is typically reduced and FVC is normal or increased. In end-stage chronic pulmonary disease, FVC may also be reduced, leading to a false normalization of the FEV1:FVC ratio44
Serum a1-antitrypsin levels should be determined for patients suspected of having a1-antitrypsin-deficiency emphysema. If emphysema is clinically evident in a young patient or in a patient without a significant smoking or occupational exposure history, a1-antitrypsin deficiency may be responsible. Phenotyping should be performed if the a1-antitrypsin level is low.
ABG levels should also be measured if there is evidence of cyanosis or cor pulmonale, or if FEV1 is less than 1 L.4 Additional diagnostic studies that may be useful are chest radiography, a sputum evaluation, a complete blood count with differential, and a baseline electrocardiogram.
Principles of Management
The general principles of patient management in COPD are based on the goals of slowing disease progression, preventing infection, treating reversible symptoms, and educating patients. The RCP is intimately involved in all four cornerstones of care.
If the extent of disease is not completely irreversible (end-stage disease), the progression of disease can be slowed through smoking cessation, reduction of exposure to environmental or occupational irritants, and therapy with supplemental oxygen.
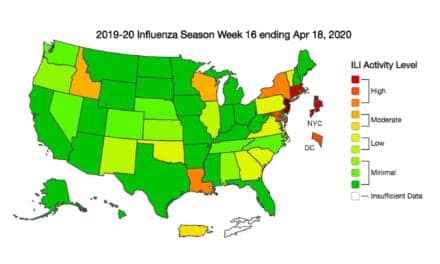
In order to prevent infection, patients with COPD should be encouraged to have annual influenza vaccinations. Some authorities also recommend vaccination against pneumococcal disease. Many bacteria and other organisms have been found in the sputum of patients with chronic pulmonary disease. These include Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus viridans, Klebsiella species, Moraxella (formerly called Branhamella) catarrhalis, Staphylococcus aureus, Staphylococcus epidermidis, and Candida albicans (a fungus). Broad-spectrum antibiotic prophylaxis has not been shown to decrease the frequency of infections, but may decrease the severity and duration of symptoms.
Pharmacotherapy with b-agonists and long-acting theophylline preparations may reverse the symptoms of airway obstruction.
Education should be an integral part of COPD management. Patients and their families should be given basic facts about the disease process and offered a list of resources, in the event that they desire additional information. Medication issues should be addressed. If appropriate, the subject of intubation and resuscitative intervention should be reviewed and the patient’s desires should be delineated.
Managing Reversible Bronchospasm
Pharmacological agents for managing reversible bronchospasm associated with COPD include theophylline, b-agonists, corticosteroids, anticholinergics, mucolytics, and, if appropriate, a1-antitrypsin.
Although theophylline has limited bronchodilation effects, it may cause improved peripheral ventilation, resulting in a fall in trapped-gas volume and an increase in exercise tolerance. It can improve mucociliary clearance and the overall work of breathing. Theophylline augments central respiratory drive and may also improve diaphragm-muscle activity and decrease vascular and pulmonary bronchiolar resistance. There is some evidence that theophylline may provide protection against episodic bronchospasm. Animal studies3,7 suggest a possible anti-inflammatory effect. Long-acting preparations taken in the early evening have the added advantages of controlling nocturnal symptoms and increasing compliance.8
Selective b2-agonists cause vasodilation of peripheral and pulmonary vessels. Cardiovascular effects include reflex tachycardia and reduction of biventricular afterload in patients with severe COPD. A major problem with potent b2-agonists is that they act on muscle receptors to accelerate the relaxation phase of slow-contracting fibers, thus producing tremor. b-agonists may improve mucociliary clearance. Tolerance may be a problem; the most common difficulty limiting the efficacy of b-agonists is inadequate dosage resulting from inefficient use. The use of inhaled b-agonists may reduce systemic effects such as tremor.3,7
Use of corticosteroids has increased, despite controversy concerning their efficacy in chronic pulmonary disease. Corticosteroids penetrate the cytoplasm of cells, bind to steroid receptors, and influence RNA sequences, thereby modulating protein synthesis. In addition, they directly influence the release of other mediators, such as leukotrienes, and thus inhibit the inflammatory process. They also interfere with neutrophil activity and block portions of the complement system.3
Anticholinergic agents are potent bronchodilators. Atropine inhibits vagal bronchospasm. Many side effects, however, preclude their routine use. Ipratropium is three to five times more potent than atropine as a bronchodilator and is poorly absorbed through the gastrointestinal tract, which minimizes systemic toxicity.3 Its onset of action is reached only slowly, though, and it must be used regularly, mitigating its use for episodic bronchospasm.3
Mucolytic agents have variable effectiveness in patients with chronic pulmonary disease. They work by liquefying mucus through hydration or by changing its chemical structure, leading to improved transport and clearance of secretions by the ciliary network in the bronchial tree. Unfortunately, agents such as ammonium chloride and guaifenesin must be given in extraordinarily large doses if they are to have any objective effect, and acetylcysteine irritates the airways of many patients.3
Replacement therapy with biosynthetic a1-antitrypsin is the primary therapy for a1-antitrypsin–deficient individuals.
Smoking cessation is perhaps the single most important nonpharmacological therapy. Usually, long-term cessation will allow for reversal of the reversible portion of obstructive disease. Supplemental oxygen may sustain arterial Po2 in late-stage or end-stage patients. Oxygen therapy may also prolong survival.9 Rehabilitation that teaches the patient to live with chronic pulmonary disease may also help improve his or her quality of life. Education is important and may increase compliance. Surgical interventions are not routinely performed. However, if surgery is performed, resection of part of the lung will leave the patient with a reduced lung volume. Such patients require careful postoperative monitoring to ensure adequate pulmonary function.
Occupational Exposures
More than 200 agents have been shown to cause occupational asthma and COPD. This number is likely to grow as new chemical agents are introduced into the workplace. Agents that cause occupational asthma include both naturally occurring and synthetic compounds.
Although the list of etiologic agents for occupational asthma is more than 200 items long and growing, only a few of these agents have been extensively studied. These include diisocyanates, epoxy resins, and wood dusts. Epoxy resins are made from acid anhydrides. They have a wide range of application for reinforced plastics, adhesives, molding resins, and surface coatings. They are potent irritants, and it is usually difficult to distinguish between allergic and irritant mechanisms. Roughly 40% of epoxy resin workers develop specific immunoglobulin E antibodies to anhydride protein, and 20% develop respiratory disease associated with the immunologic reaction.10,11
Ambient Air Pollution
In contrast to ozone, nitrogen dioxide is found at higher levels indoors than outdoors, primarily in association with the use of gas stoves and kerosene heaters. Outdoor nitrogen dioxide, however, contributes a significant fraction to indoor levels. Nitrogen dioxide is less reactive than ozone; because of its low solubility, it penetrates to the lung periphery, where more than 60% may be deposited. At peak indoor levels of nitrogen dioxide, studies of healthy volunteers have generally failed to show alterations in lung mechanics or evidence of inflammation with short-term exposure to levels of 0.5 to 2 ppm; however, animal exposure studies12 provide evidence that nitrogen dioxide exposure at similar levels impairs host defenses against bacterial challenge. Some studies12 suggest that patients with asthma, and those with mild COPD, may be particularly sensitive to the adverse effects of nitrogen dioxide on lung function.
Carbon monoxide from automobile exhaust and from second-hand cigarette smoke has been recognized as an important component of ambient air pollution. Even modest increases in carboxyhemoglobin in patients with ischemic heart disease may cause decreased exercise tolerance. Chronic elevation of carboxyhemoglobin caused by cigarette smoking in pregnant women adversely affects fetal health.
Residents of urban areas with high air pollution appear to have an increased frequency of respiratory symptoms and slightly reduced pulmonary function. Although the specific pollutants involved have not been firmly established, a causal relationship between air pollution and reduced pulmonary function seems likely.
Passive Smoke Exposure
Passive exposure to tobacco smoke as a form of environmental pollution has received considerable attention in recent years. Tager et al13 found a significant effect of maternal smoking on the rate of growth of FEV1 in children followed prospectively for 7 years. They estimated a 3% reduction in the projected FEV1 attained by a male nonsmoking child exposed to a smoking mother from ages 11 to 16, compared to the nonsmoking child of a nonsmoking mother. Subsequent studies14 of the effect of maternal smoking during pregnancy showed that in utero tobacco smoke exposure contributes to significant reductions in pulmonary function measured after birth.
Masi et al15 studied the effects of environmental tobacco-smoke exposure in young, nonsmoking adults aged 15 to 35 years. They estimated cumulative exposure using a questionnaire that assessed exposure at different ages. In men, a significant relationship between household smoke exposure and pulmonary function was demonstrated.
The deleterious effects of passive smoke exposure on adults are less defined than in infants and children, but some negative effect is likely to be present. The magnitude of the effect of environmental tobacco smoke on pulmonary function in healthy adults remains to be more fully elucidated.
Opportunities for Intervention
The RCP has an important role in the management of obstructive lung diseases. Recognition is the first step toward avoidance. By educating the patient about possible triggers associated with his or her occupation and/or environment, the RCP provides an improved opportunity for trigger identification.
Surveillance programs are a keystone of prevention. They may identify individuals who are at an increased risk for developing asthma or COPD in the workplace, and they may detect disease at an early stage, when intervention is more likely to be successful. The most sensitive health-surveillance programs currently available include pre-employment and periodic examinations, immunological monitoring, and periodic spirometric surveys.16
Cigarette smoking provides, for the smoker, the most intense exposure to pollution of any kind, and indoor smoking can contribute significantly to the exposure of other people. Measures to encourage smokers to quit, and to persuade young people not to start smoking, offer what is, perhaps, the greatest opportunity to reduce the prevalence of chronic lung disease.
Particular care is required to avoid the exposure of young children to high levels of pollution, whether of outdoor or indoor origin. Not only are there links between such exposures and the occurrence of respiratory illnesses, but these early experiences also may contribute to the development of COPD later in life.
John D. Zoidis, MD, is a contributing writer for RT Magazine.
References
1. Ferguson GT, Cherniack RM. Management of chronic obstructive pulmonary disease. N Engl J Med. 1993;328:1017-1022.
2. Fei RH, Murata GH. Contemporary management of the patient with chronic obstructive pulmonary disease. Compr Ther. 1994;20:277-281.
3. Nesse RE. Pharmacologic treatment of COPD. Optimum therapy for ambulatory patients. Postgrad Med. 1992;91:71-72, 77-78, 81-82, 84.
4. Angstman GL. Diagnosing COPD. How to identify patients with irreversible obstruction of the airways. Postgrad Med. 1992;91:61-62, 65, 67.
5. Subramanian D, Guntupalli KK. Diagnosing obstructive lung disease. Why is differentiating COPD from asthma important? Postgrad Med. 1994;95:69-70, 75-78, 83-85.
6. Thurlbeck WM. Pathophysiology of chronic obstructive pulmonary disease. Clin Chest Med. 1990;11:389-403.
7. Ziment I. Pharmacologic therapy of obstructive airway disease. Clin Chest Med. 1990;11:461-486.
8. Make B. COPD: management and rehabilitation. Am Fam Physician. 1991;43:1315-1324.
9. Hanson MA, Midthun DE. Outpatient care of COPD patients. Postgrad Med. 1992;91:89-90,93-94,96.
11. Chan-Yeung M, Malo J-L. Occupational asthma. N Engl J Med. 1995;333:107-112.
12. Committee of the Environmental and Occupational Health Assembly, American Thoracic Society. Health effects of outdoor air pollution. Am J Respir Crit Care Med. 1996;153:3-50.
13. Tager IB, Weiss ST, Munoz A, et al. Longitudinal study of the effects of maternal smoking on pulmonary function in children. N Engl J Med. 1983;309:699-703.
14. Hanrahan JP, Tager IB, Segal MR, et al. The effect of maternal smoking during pregnancy on early infant lung function. Am Rev Respir Dis. 1992;145:1129-1135.
15. Masi MA, Hanley JA, Ernst P, et al. Environmental exposure to tobacco smoke and lung function in young adults. Am Rev Respir Dis. 1988;138:296-299.
16. American College of Chest Physicians. ACCP consensus statement. Assessment of asthma in the workplace. Chest. 1995;108:1084-1117.