Over the past decade or so, asthma therapy has progressed significantly. New steroids with greater potency and long-acting b-agonists have been added to the marketplace. Medications that alter the leukotriene inflammatory pathway have provided additional tools for control of asthma symptoms. Asthma, however, continues to be a very frequent cause of illness for many patients in the United States. Indeed, data1 from 2004 showed that approximately 20 million US residents have been diagnosed with asthma; of these, 6 million were children. Having asthma as a child means that many school days are lost due to illness. It also means that many parents have to take time off work to provide care for these children. As a result of medical visits, hospitalizations, emergency-department visits, and medications, asthma accounted for $11.5 billion in direct health care costs and $4.6 billion in indirect costs in 2004.1 Due to this great need to improve treatment, basic-science research continues into the underlying mechanisms of this inflammatory illness.
Changes in the airway are well known. At the cellular level, degranulated mast cells, increased numbers of eosinophils, and a higher ratio of subtype-2 helper T cells (TH2) to TH1 lymphocytes are the primary factors involved in asthma.2 In addition, subepithelial fibrosis is a common finding in asthma, along with airway smooth-muscle hypertrophy and increased mucus-secretory cells (both individual goblet cells and mucus glands). Multiple inflammatory pathways lead to cell activation within the airway.
Activation of these inflammatory cells occurs through the action of many different cytokines (proteins secreted by white blood cells that interact with other white blood cells or other inflammatory cells). Primary cytokines felt to be involved in asthma are interleukin (IL) 4, IL-5, and IL-13.3 IL-4 is a key protein involved in differentiation of TH2 lymphocytes and attraction of eosinophils. The attraction of eosinophils into the airway is also a key role for IL-5. IL-13’s function is also to induce eosinophilia, as well as to increase mucus production and airway hyperresponsiveness after allergen challenge. Given the central role of these proteins in the allergic response in asthma, many investigators have looked at multiple ways to block their effects.
Ciclesonide
Corticosteroids have been the mainstay of therapy for asthma for many years. Research into the mechanism of action of anti-inflammatory steroids shows that they turn off genes involved in promoting inflammation and activate genes that have anti-inflammatory actions.4 Used both during acute exacerbations and as chronic medications for the control of inflammation, they have certainly proved to be effective in symptom control. As is well known, however, steroid side effects may occur in many patients. These can include oral Candida infections and dysphonia (voice alterations). More serious adverse reactions can include suppression of the immune system, cataracts, and growth suppression in children. Rarely, reports of altered behavior have been attributed to these medications, as well.
Given this background, efforts have been undertaken to create a safer steroid. One approach is to create a molecule that is only active at the intended site of action (the airway). Ciclesonide is a steroid that has been specifically synthesized for this effect.5 This new inhaled steroid is inactive when initially entering the lung. Esterases within the airway epithelium generate the active compound known as desisobutyryl-ciclesonide (des-ciclesonide).6 Once activated within the lung cell, it is a very potent steroid. A longer acting form of des-ciclesonide is made by combining it with fatty acids. This, essentially, creates a reservoir of the drug that has prolonged activity at the needed site. Little of the drug is absorbed across the mouth or pharynx, eliminating potential adverse effects there. Metabolism by the liver of any swallowed drug is nearly complete; this, again, serves to make the drug safer. When the drug is administered using a hydrofluoroalkane metered-dose inhaler, more than 50% of the drug is deposited in the lung.
Clinical trials7 with ciclesonide show good activity in controlling asthma. Several trials8,9 have compared it with inhaled budesonide, while others10 have compared it with placebo. In the budesonide trials, ciclesonide was as effective as twice-daily budesonide in increasing lung function after 12 weeks of therapy. Asthma-symptom scores also improved in both groups receiving ciclesonide and budesonide. With regard to safety, several studies11 have shown that ciclesonide had no effect on the normal daily secretion of endogenous cortisol. The same was true when urinary excretion of cortisol was measured; no effect was seen after inhalation of ciclesonide. Using very sensitive measures of bone metabolism, investigators found no inhibition of bone formation with ciclesonide. The side effects seen with use of ciclesonide were similar to those seen with inhaled budesonide. Overall, this medication shows significant promise in advancing asthma therapy.
Phosphodiesterase Inhibitors
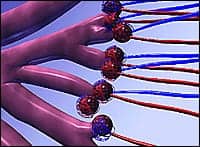
Phosphodiesterases (PDEs) are proteins that naturally regulate the levels of cyclic nucleotides.12 Eleven different families of PDEs are known. PDEs are found in many different cells throughout the body; in asthma, proteins of the PDE4 family are found in inflammatory cells (T lymphocytes, eosinophils, macrophages, and neutrophils) and airway smooth muscle.13 Inhibition of PDE4 will increase the amount of intracellular cyclic adenosine monophosphate (cAMP); increased cAMP will then lead to inhibition of inflammatory-cell function. Specifically, inhibition of PDE4 leads to a reduction in the synthesis and export of eosinophils from the bone marrow. PDE4 inhibitors will also decrease the transit of eosinophils from the circulation to the lung, along with decreasing secretion of inflammatory mediators from immune cells. In addition, this class of medicines might also decrease the release of inflammatory mediators from neutrophils, T lymphocytes, airway epithelial cells, basophils, monocytes, and macrophages. With this as their rationale, researchers have synthesized several different compounds that have reached phase-III clinical testing.
Roflumilast is a selective PDE4 inhibitor that is being tested for use in both asthma and chronic obstructive pulmonary disease (COPD). Animal experiments14 show that roflumilast is effective in inhibiting production of mast cells, eosinophils, neutrophils, lymphocytes, and macrophages and that it inhibits inflammation and airway remodeling in asthmatic rats. In allergic asthma, roflumilast was evaluated15 for activity in early-phase and late-phase drops in lung function; results demonstrated greater preservation of lung function for the late phase than the early phase when the drug was given for a week at a dose of 500 µg daily. Over a 3-month comparison of doses of 500 µg and 100 µg, roflumilast was associated with a dose-dependent increase in forced expiratory volume in 1 second (FEV1) and morning peak expiratory flow rates. This study16 involved 690 patients, varying in age from 15 to 70 years. Similar effects were seen over a 12-month follow-up period. Another trial17 compared the efficacy of roflumilast and beclomethasone in a 12-week trial. Study subjects had a 1-week to 3-week placebo run-in period. They were then given, randomly, either beclomethasone (200 µg, twice daily) or roflumilast (500 µg, once daily). Subjects in both treatment groups showed equal improvement in FEV1 and equal decreases in the use of bronchodilator medication. In addition, roflumilast has shown effectiveness in preventing exercise-induced bronchospasm.
Cilomilast is another PDE4 inhibitor investigated for activity in COPD and asthma. In vitro investigation of this molecule shows that it is effective in inhibiting eosinophil movement into the lung after antigen or leukotriene challenge.18 In animal models, it has also been found to have bronchodilatory effects and suppressive effects on cytokine production. The use of cilomilast in asthma has been assessed in a 6-week trial19 with patients already using inhaled corticosteroids whose asthma was not completely controlled. More than 300 patients were enrolled, and they received 5, 10, or 15 mg of cilomilast twice daily. In the 15-mg group, FEV1 showed sustained improvement over the course of the trial; clinical improvement was also noted within the first 4 hours of treatment, demonstrating a rapid onset of action. Other clinical indicators of pulmonary function were seen to improve significantly.
Cilomilast was also evaluated in a 12-month study20 in which statistically significant increases in FEV1, forced vital capacity, and peak expiratory flow rate were seen. Asthma symptoms (cough, wheezing, breathlessness, and chest tightness) were also improved in those on the active drug.
Asthma symptoms due to exercise have been shown to be decreased after use of cilomilast. In these studies,21 subjects received either cilomilast or placebo for 7 day. Exercise challenges were performed on days 1 and 7. Decreases in lung function were less in those who received cilomilast than in placebo-group subjects. After a week of treatment, 40% of cilomilast-group subjects had insignificant decreases in FEV1 after exercise.
As promising as both roflumilast and cilomilast appear, adverse effects may limit the usefulness of these medications.22 As they are for theophylline, gastric effects may be limiting. Summary data for cilomilast in placebo-controlled trials show that the incidence of nausea was about 15% for those being treated with the active drug, compared with about 6% for placebo-group patients. Roflumilast has also been shown to have a similar side-effect profile, with headache, nausea, diarrhea, dizziness, and sleep disturbances most commonly reported.
Summary
Multiple avenues of investigation into the mechanisms of asthma are ongoing. This research has the potential for helping to provide much better insight into this chronic respiratory illness. Improved understanding should also lead to therapies that are better than current medications used. Corticosteroids have been a standard regimen for many years; concerns for adverse events have lead to the development of ciclesonide, a novel molecule that is activated within the airway epithelium. Once activated, a depot effect of the active compound forms, so that a steady amount of medication is available to inhibit inflammation. Ciclesonide was approved for treatment of asthma in the United Kingdom and Australia in 2004; phase III trials are underway in the United States. New compounds that inhibit phosphodiesterase are also being thoroughly investigated as new potential asthma drugs. These may be thought of a vast improvements on theophylline by having significant specificity for the inflammatory cells involved in asthma. Roflumilast and cilomilast have been studied extensively for asthma and are being evaluated for submission to various regulatory authorities for marketing approval.
Christopher Harris, MD, is assistant professor of pediatrics, Division of Pediatric Pulmonary Medicine; medical director, pediatric pulmonary function laboratory; and assistant director, Cystic Fibrosis Center, Vanderbilt Children’s Hospital, Nashville.
References
1. American Lung Association.Trends in Asthma Morbidity and Mortality. Epidemiology & Statistics Unit. Research and Program Services. Available at: www.lungusa.org/atf/cf{7A8D42C2-FCCA-4604-8ADE-7F5D5E762256}/ASTHMA1.PDF. Accessed June 30, 2006.
2. Busse WW, Lemanske RF. Asthma. N Engl J Med. 2001;344(5):350-62.
3. Barnes PJ. New drugs for asthma. Nat Rev. 2004;3(10):831-44.
4. Barnes PJ, Adcock IM. How do corticosteroids work in asthma? Ann Intern Med. 2003;139:359-70.
5. Reynolds NA, Scott LJ. Ciclesonide. Drugs. 2004;64(5):511-9.
Mutch E, Nave R, Zech K, Williams FM. Eur Respir J. 2003;22(S45): Abstract P1749.
6. Reynolds NA, Scott LJ. Ciclesonide. Drugs. 2004;64(5):511-9.
7. Hansel T, Engelstätter R, Benezet O, et al. Once daily ciclesonide (80 mg or 320 mg) is equally effective as budesonide 200 mg given twice daily: a 12-week study in asthma patients. Eur Respir J. 2003; 22(suppl 45): 410s.
8. Ukena D, Biberger C, von Behren V, Malek R, et al. Ciclesonide significantly improves pulmonary function when compared with budesonide: a randomized 12-week study. Eur Respir J. 2003;22(suppl 45):411s.
9. Chapman KR, D’Urzo AD, Oedekoven C, et al. Effects of ciclesonide versus placebo on lung function after 12 weeks of treatment in patients with asthma. Am J Respir Crit Care Med. 2002;165(8 pt 2):A767.
10. Weinbrenner A, Huneke D, Zschiesche M, et al. Circadian rhythm of serum cortisol after repeated inhalation of the new topical steroid ciclesonide. J Clin Endocrinol Metab. 2002;87(5):2160-3.
12. Spina D. Phosphodiesterase-4 inhibitors in the treatment of inflammatory lung disease. Drugs. 2003;63(23):2575-94.
13. Chung KF. Phosphodiesterase inhibitors in airways disease. Eur J Pharmacol. 2006; 533:110-7.
14. Karish SB, Gagnon JM. The potential role of roflumilast: the new phosphodiesterase-4 inhibitor. Ann Pharmacother. 2006;40: 1096-1104.
15. van Schalkwyk EM, van Heerden K, Bredenbröker D, et al. Dose-dependent inhibitory effect of roflumilast, a new, orally active selective phosphodiesterase 4 inhibitor, on allergen-induced early and late asthmatic reaction. Eur Respir J. 2002;20 (suppl 38):110s.
16. Leichtl S, Schmid-Wirlitsch C, Bredenbröker D, et al. Roflumilast, a new, orally active, selective phosphodiesterase 4 inhibitor, is effective in the treatment of asthma. Eur Respir J. 2002;20(suppl 38): 303s.
17. Albrecht A, Leichtl S, Bredenbröker, et al. Comparison of roflumilast, a new, orally active, selective phosphodiesterase 4 inhibitor, with beclomethasone diproprionate in asthma control. Eur Respir J. 2002;20 (suppl 38):304s.
18. Down G, Siederer S, Lim S, Daley-Yates P. Clinical pharmacology of Cilomilast. Clinical Pharmacokinetics. 2006;45(3): 217-33.
19. Compton C, Cedar E, Nieman RB, et al. Ariflo improves pulmonary function in patients with asthma: results of a study in patients taking inhaled corticosteroids. Am J Respir Crit Care Med. 1999;159:A624.
20. Compton C, Duggan M, Cedar E, Nieman RB, et al. Ariflo efficacy in a 12-month study of patients with asthma. Am J Respir Crit Care Med. 2000;161: A505.
21. Nieman RB, Fisher BD, Amit O, Dockhorn RH, et al. SB207499 (Ariflo™), a second-generation, selective oral phosphodiesterase type 4 (PDE4) inhibitor, attenuates exercise induced bronchoconstriction in patients with asthma. Am J Respir Crit Care Med. 1998;157:A413.
22. Huang Z, Ducharme Y, Macdonald D, Robichaud A. The next generation of PDE4 inhibitors. Curr Opin Chem Biol. 2001; 5(4):432-8.









