The general principles of managing patients with COPD are to slow disease progression, to prevent infection, to treat reversible symptoms, and to educate patients. The RT is intimately involved in all four cornerstones of care.

Pathophysiology and Risk Factors
COPD is a disease in which cigarette smoke causes an overproduction of the enzyme elastase, one of the immune system’s infection-fighting biochemicals. This results in irreversible destruction of the protein elastin, which is important for maintaining the structure of the walls of the alveoli. As the walls of the alveoli rupture, the number of alveoli is reduced and many of those remaining are enlarged, making the lungs of the patient with COPD overinflated and less elastic. Due to the higher pressure inside the chest that must be developed to force air out of the less elastic lungs, the bronchioles tend to collapse during exhalation. Stale air becomes trapped and fresh air cannot replace it.
Cigarette smoking is undeniably the most important risk factor for COPD, implicated in more than 90% of all cases. Cigar and pipe smoking can also contribute to COPD. Air pollution and industrial dusts and fumes are other important risk factors. Family clustering has also been identified as a risk factor; it is thought that heredity predisposes people in certain families to the development of COPD when other causes, such as smoking and air pollution, are present. Lung infections can make all forms of COPD worse, and are therefore considered a risk factor.
In the general population, COPD usually develops in older individuals with a long smoking history. There is, however, a form of COPD that is seen in families. People with this type of COPD have a hereditary deficiency of the enzyme inhibitor a1-antitrypsin (AAT). This type of COPD is sometimes called early-onset COPD because it can appear in a person as young as 30 years old.
AAT is a serum protein that is produced in the liver. It functions to protect the lungs so they can work normally. The destruction of elastin that occurs in COPD is believed to result from an imbalance between two proteins in the lung: elastase, which breaks down elastin, and AAT, which inhibits elastase. In healthy people, there is usually enough AAT to protect elastin so that abnormal elastin destruction does not occur. When there is a genetic deficiency of AAT, however, the activity of the elastase is not inhibited, and elastin breakdown occurs.
AAT deficiency is an autosomal codominantly inherited disorder occurring in about 1 in every 3,000 births.6 Carrying the trait does not invariably lead to the disease. Each parent must contribute one abnormal gene to produce a child with AAT deficiency. It is estimated that 1% to 3% of all cases of COPD are due to AAT deficiency.7
If individuals with AAT deficiency smoke, they may exhibit symptoms of COPD by the time they reach early middle age. People from families in which relatives have developed COPD in their 30s and 40s should be tested for AAT deficiency. If a deficiency is found, it is especially important for the individual not to smoke.
Advances in the understanding of AAT deficiency have led to the establishment of clinical criteria that may lead to the identification of this disorder in some individuals with early symptoms of COPD. There are several options for treatment of AAT deficiency, including replacement of the missing protein.
Clinical Manifestations
The preclinical course of patients with COPD is highly variable. Patients with a history of lung disease early in life may exhibit reduced pulmonary function in adulthood. Smoking in patients with a history of childhood lung disease may lead to a progressive decline in lung function. Other patients who smoke probably begin adulthood with normal lung function. Forced expiratory volume in 1 minute usually remains within normal limits until middle age, when a rapid decline in pulmonary function ensues. Generally, this decline stops in patients who quit smoking. The clinical symptoms of COPD typically will appear in patients who continue to smoke.
In general, emphysema is characterized pathophysiologically by permanent abnormal airspace enlargement and loss of elasticity.8 This enlargement occurs distal to the terminal bronchioles, and is associated with destruction of the airspace walls. Chronic bronchitis is characterized by chronic cough, sputum production, and inflammation of the mucosal surfaces of the larger airways.
Patients with COPD usually present with shortness of breath, cough, and/or wheezing. Coughing usually indicates excess mucus production. The shortness of breath is a result of increased work of breathing through obstructed airways, and is usually initially associated with increasing levels of exertion. Over time, the dyspnea worsens to the point of occurring at rest. Wheezing occurs as a result of airway narrowing, mucosal edema, and retained secretions. Often, patients with COPD have been described as either blue bloaters or pink puffers. Blue bloaters have central cyanosis with secondary polycythemia and edema. Arterial blood gas evaluation usually reveals evidence of hypoxemia (PO2 of 45 to 55 mm Hg), carbon dioxide retention (PCO2 of 50 to 60 mm Hg), and compensated respiratory acidosis (pH of 7.38 to 7.42).9 Pink puffers do not have secondary polycythemia, and edema is not present. They have less hypoxemia (PO2 of 60 to 80 mm Hg) and no carbon dioxide retention (PCO2 of 30 to 40 mm Hg).9 Many patients have features of both conditions.
Principles of Management
The general principles of managing patients with COPD are to slow disease progression, to prevent infection, to treat reversible symptoms, and to educate patients. The RT is intimately involved in all four cornerstones of care. If the extent of disease is not yet at a point of complete irreversibility (end-stage COPD), the progression of disease can be slowed by smoking cessation, reduction of exposure to environmental or occupational irritants, and therapy with supplemental oxygen.
Patients with COPD should be encouraged to have annual influenza vaccinations. Some authorities also recommend vaccination against pneumococcal disease. Many bacteria and other organisms have been found in the sputum of patients with COPD. These include Haemophilus influenzae, Streptococcus pneumoniae, Streptococcus viridans, Klebsiella species, Moraxella (formerly called Branhamella) catarrhalis, Staphylococcus aureus, Staphylococcus epidermidis, and Candida albicans (a fungus). Broad-spectrum antibiotic prophylaxis has not been shown to decrease the frequency of infections, but may decrease the severity and duration of symptoms.
Pharmacotherapy with b-agonists and long-acting theophylline preparations may reverse the symptoms of airway obstruction, and additional medications are also useful.
Education should be an integral part of COPD management. Patients and their families should be given basic facts about the disease process and offered a list of sources of additional information. Medication issues should be addressed. If appropriate, intubation and resuscitative intervention should be discussed and the patient’s desires should be delineated.
Drug Therapy
Pharmacological agents for managing reversible bronchospasm associated with COPD include theophylline, b-agonists, corticosteroids, anticholinergic agents, mucolytic agents, and, if appropriate, AAT.
Although theophylline has limited bronchodilator effects, it may cause improved peripheral ventilation, resulting in a fall in trapped gas volume and an increase in exercise tolerance. It can improve mucociliary clearance and the overall work of breathing. Theophylline augments central respiratory drive and may also improve diaphragm muscle activity and decrease vascular and pulmonary bronchiolar resistance. There is some evidence that theophylline may provide protection against episodic bronchospasm. Animal studies10 suggest a possible anti-inflammatory effect. Long-acting preparations taken in the early evening have the added advantages of controlling nocturnal symptoms and increasing compliance.11
Selective b2-agonists cause vasodilation of peripheral and pulmonary vessels. Cardiovascular effects include reflex tachycardia and reduction of biventricular afterload in patients with severe COPD. A major problem with potent b2-agonists is that they act on muscle receptors to accelerate the relaxation phase of slow-contracting fibers, thus producing tremor. b-Agonists may improve mucociliary clearance, but tolerance may be a problem. The most common difficulty limiting the efficacy of b-agonists is inadequate dosage resulting from inefficient use. The use of inhaled b-agonists may reduce the incidence of systemic effects such as the tremor.
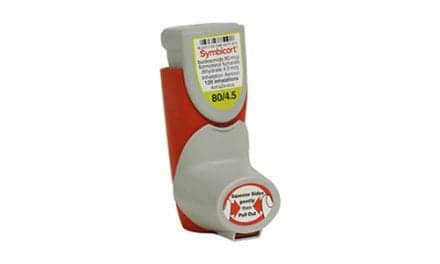
Inhaled b2-agonist bronchodilators are used either for the relief of acute respiratory distress (as needed) or for long-term maintenance. Agents with a rapid onset of action (such as albuterol) are used to relieve acute distress, and those with a long duration of action (such as salmeterol) are used for maintenance. One inhaled b2-agonist (formoterol) is a highly selective b2-agonist bronchodilator that has a unique combination of rapid-onset bronchodilation (within 1 to 3 minutes) and a long duration of action (more than 12 hours).
Use of inhaled corticosteroids has increased, despite controversy about their efficacy in COPD. Corticosteroids penetrate the cytoplasm of cells, bind to steroid receptors, and influence RNA sequences, thereby modulating protein synthesis. In addition, they directly influence the release of other mediators, such as leukotrienes, thereby inhibiting the inflammatory process. They also interfere with neutrophil activity and block portions of the complement system.
While the presence of inflammatory changes in the airways of patients with COPD provides a rationale for the use of corticosteroids, the association between these changes, lung function, and the therapeutic response to corticosteroids has not yet been established clearly. For example, whether a response to 30 mg of prednisolone over 2 weeks predicts an ongoing improvement with inhaled corticosteroid treatment is debatable, and results are awaited from ongoing studies.
Anticholinergic agents are potent bronchodilators. Atropine inhibits vagal bronchospasm, but many side effects preclude its routine use. Ipratropium is three to five times more potent than atropine as a bronchodilator and is poorly absorbed through the gastrointestinal tract, which minimizes systemic toxicity. Its onset of action is slow, however, and it must be used regularly, mitigating use for episodic bronchospasm.
Mucolytic agents have variable effectiveness in patients with COPD. They work by liquefying mucus through hydration or by changing its chemical structure, leading to improved transport and clearance of secretions by the ciliary network in the bronchial tree. Unfortunately, agents such as ammonium chloride and guaifenesin require extraordinarily large doses for any objective effect, and acetylcysteine irritates the airways of many patients.
Replacement therapy with biosynthetic AAT is the primary therapy for AAT–deficient individuals.
Other Treatments
Surgical procedures for COPD are rare, expensive, and often not covered by insurance. Most patients cannot be helped by surgery, and no single procedure is ideal for those who can be helped.
Smoking cessation is perhaps the single most important nonpharmacological therapy. Usually, long-term cessation will allow for reversal of the reversible portion of obstructive disease.
Rehabilitation, designed to help patients learn how to live with chronic pulmonary disease, may assist patients in maintaining quality of life for a prolonged period. A structured, outpatient pulmonary rehabilitation program improves functional capacity in certain patients with COPD.
Prognosis and Intervention
COPD is a disease that can be treated and controlled, but not cured. Survival of patients with COPD is clearly related to their lung-function levels at the time of diagnosis and the rate at which they lose lung function. For patients with COPD who have lost approximately two thirds of lung function at diagnosis, the median survival time is about 10 years.12
Interventional measures will be required in order to quell the coming COPD epidemic. The RT, in particular, has an important role in the management of COPD. Educational measures to encourage smokers to quit (and young people not to start smoking in the first place) offer, perhaps, the greatest opportunity for reducing the prevalence of COPD.
Surveillance programs are a keystone of prevention. They may identify individuals at increased risk for developing COPD in the workplace, and may also detect disease at an early stage, when intervention is likely to be successful. The most sensitive health surveillance programs currently available include pre-employment and periodic examinations, immunological monitoring, and periodic spirometric surveys.
Particular care is required to avoid the exposure of young children to high levels of pollution, whether of outdoor or indoor origin. Not only are there links between such exposures and the occurrence of respiratory illnesses, but these early experiences also may contribute to the development of COPD later in life.
John D. Zoidis, MD, is a contributing writer for RT.
References
1. Ferguson GT, Cherniack RM. Management of chronic obstructive pulmonary disease. New Engl J Med. 1993;328:1017-1022.
2. Halbert RJ, Isonaka S, George D, Iqbal A. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest. 2003;123:1684-1692.
3. Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121:121S-126S.
4. Stang P, Lydick E, Silberman C, Kempel A, Keating ET. The prevalence of COPD: using smoking rates to estimate disease frequency in the general population. Chest. 2000;117:354S-
359S.
5. Subramanian D, Guntupalli KK. Diagnosing obstructive lung disease. Why is differentiating COPD from asthma important? Postgrad Med. 1994;95:69-70,75-78,83-85.
6. Silverman EK, Chapman HA, Drazen JM, et al. Genetic epidemiology of severe, early-onset chronic obstructive pulmonary disease. Risk to relatives for airflow obstruction and chronic bronchitis. Am J Respir Crit Care Med. 1998;157:1770-1778.
7. Eden E, Mitchell D, Mehlman B, et al. Atopy, asthma, and emphysema in patients with severe alpha-1-antitrypsin deficiency. Am J Respir Crit Care Med. 1997;156:68-74.
8. Thurlbeck WM. Pathophysiology of chronic obstructive pulmonary disease. Clin Chest Med. 1990;11:389-403.
9. Angstman GL. Diagnosing COPD. How to identify patients with irreversible obstruction of the airways. Postgrad Med. 1992;91:61-62,65,67.
10. Boner AL, Piacentini GL, Peroni DG, et al. Theophylline inhibition of BCG-induced pulmonary inflammatory responses. Ann Allergy. 1990;64:530-535.
11. Make B. COPD: management and rehabilitation. Am Fam Physician. 1991;43:1315-1324.
12. Goel A, Pinckney RG, Littenberg B. APACHE II predicts long-term survival in COPD patients admitted to a general medical ward. J Gen Intern Med. 2003;18:824-830.