Arterial blood gas analysis is a valuable tool for assessing respiratory and metabolic dysfunction. A variety of techniques, with which the technician should be aware, are available

ABG sampling is typically performed using direct arterial puncture with a specialized ABG syringe, with the sample usually taken from the radial artery. Alternative sites include the brachial artery, dorsalis pedis artery, or femoral artery. In the intensive care unit, the radial artery is commonly sampled multiple times throughout the patient’s stay, using an indwelling arterial cannula. Prior to sampling, the patient should be in a steady state (resting for at least 5 minutes). For single arterial punctures, the site is sterilized and is sometimes anesthetized using lidocaine. It is important that the technician be well trained in the procedure and use correct sampling technique. Further, if the radial artery is the selected sampling site, an Allen test1 may be helpful prior to the puncture.
Once the sample has been obtained, the needle should be blocked from room-air entry and the syringe should be placed on ice immediately. The sample should be introduced into a calibrated blood-gas analyzer.2-4 Duplicate or triplicate measurements are recommended, and agreement of results should be reviewed and evaluated. Ideally, ABG analysis should be performed on two different calibrated analyzers and the results should be compared. Arterial blood can also be evaluated using a CO-oximeter.
Noninvasive Measures
At present, two noninvasive options are available for tracking oxygen and/or carbon dioxide levels. They are pulse oximetry and transcutaneous monitoring.5 Each has benefits and limitations. Since ABG analysis is the gold standard and yields much more complete information, the noninvasive methods refer to the ABG results.5 Oximetry has been refined during the past 3 decades and yields fairly reliable results. Carboxyhemoglobin remains a primary interfering variable, creating falsely high pulse-oximetry oxygen-saturation (Spo2) readings.6
While various infrared frequencies have been used to eliminate carboxyhemoglobin interference, the actual Spo2 reading may be falsely high in patients with elevated carboxyhemoglobin or hemoglobin variants. A second consideration is adequate perfusion of the measurement site. Probe warming was attempted with limited success, better site preparation has been strongly advocated, and attempts to use vasodilating creams have met with limited success. If trending of Spo2 is desired, and the value is correlated with, and anchored to, the ABG analysis, the technique becomes very suitable and can reveal a wealth of uniquely valuable clinical information.
Transcutaneous Spo2 and Pco2 monitoring has become common in neonatal and pediatric units worldwide.7 This instrument, in this cohort, is extremely valuable, owing its existence to the permeability of the skin and the proximity of the microvascular circulation to the surface in the newborn and young. Transcutaneous monitoring is not very useful in adults because perfusion is decreased and the diffusion pathway is inhibited by dead skin cells and thicker skin compartments, as well as other barriers and limitations. Neither of the noninvasive approaches addresses acid-base status, a unique feature of ABGs in diagnosing and directing therapy.
Hypoxemia
Hypoxemia is a major medical problem because it is a common occurrence in cardiopulmonary diseases, neuromuscular disorders, and many other conditions. Rapid identification and correction are essential to prevent irreversible organ damage. Hypoxemia is associated with five basic mechanisms: inadequate inspiratory oxygen, hypoventilation, shunting, defective diffusion pathways in the lung, and ventilation-perfusion inequality. Often, the exact cause of hypoxemia is not readily identifiable because multiple mechanisms contribute to the clinical picture. ABGs provide not only Pao2 and arterial oxygen saturation but also the Paco2 and acid-base status, generating a pattern that will help clinicians in diagnosis and in the establishment of a treatment plan. Rapid ABG analysis can assist the clinician in evaluating hypoxemia, but direct measurement alone is not enough to distinguish the exact cause and help define the most appropriate therapeutic pathway. It is important to identify the underlying cause of the ABG abnormality, rather than simply correcting the hypoxemia.
To establish hypoventilation’s contribution to hypoxemia, the alveolar-arterial difference in oxygen partial pressure (Pao2-Pao2) has been used with success, yet it cannot differentiate among diffusion abnormalities, ventilation-perfusion inequality, and shunting. Further, the Pao2-Pao2 is sensitive to changes in the fraction of inspired oxygen (FIo2) and is not a good indicator of gas exchange. Normal values for Pao2-Pao2 in the young are less than 10 mm Hg, increasing to 10 to 20 mm Hg in the elderly. Another index, the arterial-alveolar oxygen-tension ratio, was derived to account for a changing FIo2. This index does not add to the established indices for evaluation of hypoxemia, but it does provide a simple method for estimating the FIo2 required to obtain a desired Pao2. In addition, this rather simple index has also demonstrated good utility in predicting shunt fraction, and it is an indicator of gas exchange at an FIo2 of 50% or more and a Pao2 of 100 mm Hg or less.8
If pulmonary shunting is suspected, calculation of the physiological shunt can be performed by dividing alveolar minus arterial oxygen content by alveolar minus mixed-venous oxygen content. The normal shunt fraction is typically less than 5% overall. Anatomical shunt is estimated using the physiological equation while the patient is breathing 100% oxygen. An arterial blood sample is obtained following 15 minutes of 100%-oxygen breathing to wash out nitrogen from the communicating lung. This practice eliminates ventilation-perfusion inequalities as the cause of an increased Pao2-Pao2 gradient. A drawback to this technique is the failure of nitrogen to be washed out from the slowly ventilated acinar units; this may not be a practical tool in patients with airway obstruction. Alternatively, anatomical shunt can be evaluated through a nuclear-medicine study using radiolabeled albumin.
Assessment of ventilation-perfusion inequality, which is the most common cause of hypoxemia, has been approached using a variety of techniques. They range from radiolabeled isotope techniques to the multiple inert-gas technique.9,10 While the latter technique is perhaps best for assessing ventilation-perfusion inequality, the procedure is complicated, expensive, time-consuming, and technically challenging. Therefore, most centers rely on ventilation-perfusion scanning techniques in the nuclear medicine laboratory.11
To evaluate a patient for maldistribution of ventilation, multiple techniques have been offered:
• multiple-breath nitrogen washout,
• phase III and IV of a single-breath nitrogen expiration,
• scanning with radioactive gas and radiolabeled aerosols,
• frequency dependence of compliance, and
• volume difference for total lung capacity measurement between single-breath (during DLCO measurement) and multiple-breath measurements (plethysmography).12
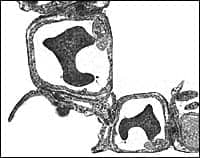
The multiple-breath nitrogen washout is the oldest and perhaps the most sensitive technique, yet it is time-consuming. The single-breath nitrogen slope is easier and less cumbersome. The single-breath tracing is divided into four phases of gas exchange: phase I is emptying of anatomical dead space, phase II is transition in emptying bronchial and bronchiolar compartments, phase III is alveolar emptying, and phase IV is the result of airway closure in the dependent parts of the lung (reflecting the inter-regional pattern of lung emptying or closing volume). The closing volume may, in some cases, exceed the expiratory reserve volume, indicating that some airways are closing during normal tidal breathing (as in severe obesity), with some degree of hypoxemia noted. Further, closing volume will increase with age due to a loss in lung elasticity (the altered elastin/collagen matrix of the lung). Xenon 133 studies are therefore employed to evaluate ventilation-perfusion differences and to identify regional areas of interest that may affect surgical or medical decisions.
Hypercapnia
The underlying physiological explanation for an increasing Paco2 is the same as that for a decreasing Pao2, with a difference in the patient’s response to the same triggers. The explanations for this difference are that oxygen and carbon dioxide are carried differently in the blood and that carbon dioxide passes more easily across the alveolar-capillary membrane. Carbon dioxide is carried in three forms: dissolved, as bicarbonate, and combined with proteins; oxygen is completely reliant on hemoglobin for transport.
The carbon dioxide¬dissociation curve is steeper and more linear than the oxygen-dissociation curve. Thus, changes in carbon dioxide are more dependent on, and reflective of, ventilation. Most notable is the ability of hyperventilation to lower Paco2 effectively without increasing Pao2 appreciably. Hypercapnia is considered a hallmark of respiratory-pump failure, not a quality index of gas exchange.
There is a definite carbon dioxide set point that the body maintains by increasing or decreasing ventilation. At high elevations and altitudes, in response to low Pao2, increased ventilation is required to maintain arterial oxygenation. This adaptive hyperventilation lowers the carbon dioxide set point.
Hypercapnia is defined as a Paco2 of 45 mm Hg or more at sea level. Altitude/elevation, however, should be considered in interpreting Paco2. The first step is to establish whether the hypercapnia is acute or chronic. Tools such as the Henderson-Hasselbach equation and nomograms can be helpful. In acute hypercapnia, for each increase in Paco2 of 10 mm Hg, pH should decrease by 0.08 units from its normal baseline value (7.4) and serum bicarbonate should decrease by 1 mEq per L. In chronic hypercapnia, the same Paco2 increase may result in a pH drop of about 0.03 units and a serum bicarbonate increase of 3.5 mEq per L. If acute and chronic hypercapnia are superimposed, the pH and bicarbonate levels will probably fall somewhere between the values typical of the purely acute and purely chronic states.
Hypercapnia may be due either to the inability to increase or maintain minute ventilation or to an impairment of the ventilatory control of breathing. These two conditions can be differentiated by drawing an ABG sample during the end of a voluntary hyperventilation effort. Further, ventilation-perfusion inequality can exacerbate hypercapnia, since the amount of minute ventilation necessary to normalize Paco2 is higher; some patients may be unable to compensate by increasing ventilation to meet the higher demand.
Acid-Base Balance
The pH of extracellular and intracellular fluids can profoundly affect the rate of metabolic reactions and enzymatic processes essential for life.13 Acid-base balance is regulated renally by adjustment of the bicarbonate level and through the respiratory control of the carbon dioxide level. All other buffer systems adjust in unison and respond to changes in bicarbonate and Paco2.14
A changing Paco2 alters pH in a rapid, direct manner. The body is capable of excreting about 12,000 mEq per day of acid in the form of carbon dioxide, compared with 100 mEq of fixed acids handled by the kidneys. Paco2 varies inversely with alveolar ventilation and directly with carbon dioxide production. Thus, ventilation has the most immediate control over pH. Metabolic acidosis is compensated for by an increase in ventilation (essentially, blowing off carbon dioxide). Likewise, metabolic alkalosis is compensated for by a decrease in ventilation and the retention of carbon dioxide. Changes in bicarbonate, Paco2, pH, Pao2, or stimuli from pulmonary mechanoreceptors alter minute ventilation and, as a result, Paco2 and pH.
The metabolic response to respiratory variations is much slower. Respiratory acidosis and alkalosis are compensated for by the kidneys’ secretion of more or less bicarbonate.15 The renal system responds slowly, with maximal excretion achieved after 7 to 10 days. Bicarbonate is turned over rapidly, however, and may be generated with carbon dioxide or lost with carbon dioxide excretion. The renal system also regulates pH by excreting hydrogen ions, ammonia, and titratable acids and through bicarbonate resorption. The ability of the renal system to resorb bicarbonate is greatest in the proximal tubule (which resorbs 85% to 90%), with additional bicarbonate resorption taking place in the distal tubule. Urinary titratable acid is formed by the conversion of monohydrogen phosphate to phosphate in the nephron. Ammonia is synthesized throughout the nephron, with 30 to 50 mmol of hydrogen ions excreted as ammonia; this excretion can increase to 300 mmol per day in severe acidosis.
Acid-base defects are classified as either metabolic or respiratory. Three parameters are necessary to describe an acid-base defect: pH, Paco2, and bicarbonate (the metabolic component).3,16-18 While pH and Paco2 can be measured directly, bicarbonate concentration is estimated using the Henderson-Hasselbach equation.14
The etiology of fully compensated acid-base abnormality is not always immediately apparent. Compensated metabolic acidosis (reduced bicarbonate) with respiratory compensation (reduced Paco2) might easily be interpreted as respiratory alkalemia with metabolic compensation. Most acid-base changes, however, may not be compensated for completely; there is a tendency toward either alkalemia or acidemia. When acid-base data are coupled with Pao2 and Paco2 (Table 3), the clinical picture may be clarified.


Respiratory acidosis may be the result of hypoventilation or ventilation-perfusion mismatching and is characterized by a rise in arterial Paco2. In acute respiratory acidosis, there is a decrease in pH, and the hydrogen-ion concentration rises in a linear fashion with the Paco2. In chronic respiratory acidosis (chronic hypoventilation), the kidney compensates by excreting hydrogen ions and generating more bicarbonate. Therefore, in well-compensated, chronic respiratory acidosis, there will be a nearly normal pH, an elevated Paco2, an increase in plasma bicarbonate concentration, an increase in total carbon dioxide, and a positive base excess. Respiratory acidosis can often be attributed to four main disorders: chronic obstructive lung disease; severe restrictive lung disease; trauma to the respiratory center, anesthesia, or other CNS depression; or neuromuscular disorders.
Respiratory alkalosis is characterized by decreased Paco2 secondary to hyperventilation. In acute hyperventilation, there is a linear relationship between a higher hydrogen-ion concentration and a lower Paco2. In chronic hyperventilation, plasma bicarbonate is decreased, which enables the pH to return to normal. Respiratory alkalosis can be caused by severe hypoxemia; metabolic acidosis; and excitement, anxiety, or other CNS-related conditions. A principal cause of hypocapnia is hypoxia: type I respiratory failure (hypoxemia with a low or normal Paco2). An ABG test will reveal a decreased Pco2, elevated hydrogen ions, decreased bicarbonate (compensatory change), and low total carbon dioxide, with an increased pH and negative base excess.
Metabolic acidosis is characterized by an increase in plasma hydrogen ions, which reduces the effective plasma bicarbonate concentration (and, therefore, pH). The decreasing pH stimulates ventilation so that carbon dioxide is removed, thereby reducing the Paco2 in the arterial blood (hyperventilation). Metabolic acidosis can have multiple causes, including diarrhea, renal failure, carbonic anhydrase inhibitors, diabetic ketoacidosis, ammonium chloride administration, anaerobic metabolism and lactic acidosis secondary to tissue hypoxia or severe exercise, hydrochloride administration, and ethylene glycol (antifreeze) or paraldehyde ingestion.15 Metabolic acidosis results from the pathophysiological derangement of generating noncarbonic acid (lactate, oxalate, or hydrochloride) or abnormal loss of bicarbonate. ABG analysis reveals a pH of less than 7.36, a Paco2 of more than 35 mm Hg, and a calculated bicarbonate of less than 18 mmol per L. The anion gap may be increased, indicating accumulation of unmeasured acid anions.
Lactic acidosis may be the result of excessive production of lactate or a reduction in the metabolism of lactic acid. It is classified as either type A (severe exercise, cardiac arrest, shock, hypoxemia, and similar causes), in which adequate oxygen delivery to tissues is compromised, or type B (thiamine deficiency, diabetes, hepatic failure, renal failure, infection, pancreatitis, and similar causes), in which tissue hypoxia does not appear to play a major role.
Renal tubular acidosis results from excess loss of urinary bicarbonate, a normal anion gap, and an elevated serum level of chlorine. It may be described as proximal or distal, depending on the renal tubular site of the defect.
Metabolic alkalosis is characterized by an increase in plasma bicarbonate concentration. The compensatory mechanism is hypoventilation, retention of carbon dioxide by the lungs. A rising Paco2 is typically on the order of 5 to 10 mm Hg, but may exceed 70 mm Hg in severe situations. Metabolic alkalosis results from loss of acids from the upper gastrointestinal tract (vomiting or gastric suction); diuretic therapy; chronic renal failure; severe potassium depletion or mineralocorticoid excess with potassium depletion; oral administration of antacids, ion-exchange resins, milk alkali syndrome, or oral bicarbonate; parenteral administration of alkali (citrate in blood transfusions or bicarbonate in severe metabolic acidosis; or excessive corticosteroids (hypersecretion in disease or steroid therapy). Metabolic alkalosis is characterized by pathophysiological derangements in which excess bicarbonate is generated or there is an abnormal loss of noncarbonic acid. Typically, the ABG analysis will depict a pH of more than 7.4, a Paco2 of more than 45 mm Hg, and bicarbonate of more than 32 mmol per L.
Anion Gap
Blood and other body fluids contain a variable number of ions, but, the total number of anions (negative ions) and of cations (positive ions) is the same because the serum is electroneutral. Ions typically measured in the blood are the cations like sodium and potassium and the anions including chlorine and bicarbonate. There are unmeasured ions in each group that contribute to the overall ionic makeup of blood. Cations typically outnumber the anions by about 8-16 mmol/L mainly because the unmeasured anions constitute a significant proportion of the total number of anions in the blood and include proteins, sulfates, phosphates, lactate, and ketones. Anion gap is the difference between the measured cations and measured anions. It is estimated by subtracting the sum of chloride and bicarbonate from the sodium concentration.
A decreased anion gap may result from hypoalbuminemia and severe hemodilatation, and rarer causes might include increased calcium and magnesium. A raised anion gap may result from dehydration and any cause for raised unmeasurable anions, like lactate, ketones, and renal acids or accompanying treatment with drugs given as organic acids such as penicillin and salicylates. Poisoning with methanol, ethanol, and paraldehyde is known to raise the anion gap.
When acids are increased in the blood, the anion gap is increased and there is a reduction in serum HCO3– that matches the anion gap. If this is not observed, a second acid-base disorder should be considered. When metabolic acidosis and alkalosis coexist (vomiting, ketoacidosis), the plasma HCO3– may be normal and the increased anion gap may indicate an underlying acid-base disturbance. To differentiate between the many causes of an increased anion gap metabolic acidosis, osmolar gap is reported and compared to the calculated osmolarity.
We can also encounter a normal anion gap metabolic acidosis. This results from the loss of alkali (HCO3-) or metabolic equivalent (excretion of salts of organic ions in proportion to excess of chloride), or an accumulation of HCl or metabolic equivalent (NH4Cl and chloride salts of amino acids). Gastrointestinal causes or renal excretion may decrease HCO3– or in surgical cases the cause is usually known.
Summary
ABG analysis is a highly valued tool for assessing respiratory and metabolic dysfunction and acid-base equilibrium and for monitoring patient status and response to therapy. If arterial blood sampling is required, the technician should be well trained in patient preparation, sampling techniques, and analysis to ensure that the results are accurate and not contaminated by venous blood, atmospheric air, or ongoing metabolic activity in the arterial specimen. Extreme care should be devoted to quality control of the analyzers and verification of accuracy many times a day, and for all shifts. Each blood-gas analyzer should be part of an ongoing quality-control program, and output should be continually scrutinized for pattern shifts suggestive of electrode dysfunction or other subtle instrumentation malfunction or drift. ABG results should be interpreted in light of the rest of the diagnostic data and clinical findings. Interpretation should include respiratory and renal contributions and a determination of whether the changes are acute or chronic (compensatory). ABG analysis should be performed periodically to monitor the efficacy of treatment and to evaluate the possibility of comorbid influences. The results of an ABG analysis are not the final answer; they are part of a dynamically changing clinical picture.
Rick Carter, MBA, PhD, is professor and chair, Department of Health, Exercise and Sport Sciences; James S. Williams, PhD, is associate professor, Department of Health, Exercise and Sport Sciences, and adjunct associate professor of physiology; Jacalyn McComb, PhD, is professor of health, exercise, and sport sciences and adjunct professor, pharmacology; and Robert Sawyer, PhD, is assistant professor, health, exercise and sport sciences, Texas Tech University, Lubbock. Brian Tiep, MD, is medical director, Respiratory Disease Management Institute, Pomona, Calif.
References
1. Cherniack RM. Pulmonary Function Testing. Philadelphia: WB Saunders; 1977.
2. Olszowka AJ, Rahn H, Farhi LE. Blood Gases: Hemoglobin, Base Excess and Maldistribution. Philadelphia: Lea and Febiger; 1973.
3. Gabel RA. Algorithms for calculating and correcting blood-gas and acid-base variables. Respir Physiol. 1980;42:211-232.
4. Driskol P, Brown T, Gwinnutt C, Wardle T. A Simple Guide to Blood Gas Analysis. 2nd ed. London: BMJ Publishing Group; 2000: 37-149.
5. Nelson CM, Murphy EM, Bradley JK, Durie RH. Clinical use of pulse oximetry to determine oxygen prescriptions for patients with hypoxemia. Respir Care. 1986;31:673-680.
6. Tiep B, Carter R, Hoffman L, Zielinski J. Management of stable COPD: long-term oxygen therapy. In: Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932-46.
7. Slagsvold CE, Stranden E, Rosen L, Kroese AJ. The role of blood perfusion and tissue oxygenation in the postischemic transcutaneous PO2 response. Vasc Surg. 1994;28:115-121.
8. Gowda MS, Klocke RA. Variability of indices of hypoxemia in adult distress syndrome. Crit Care Med. 1997;25:41-45.
9. Wagner PD. Ventilation-perfusion matching during exercise. Chest. 1992;101: 192S-198S.
10. Wagner PD, Saltzman HA, West JB. Measurement of continuous distributions of ventilation-perfusion ratios: theory. J Appl Physiol. 1974;37:588-599.
11. Milic-Emili J. Topographical inequality of ventilation. In: Crystal R, West JB, eds. The Lung: Scientific Foundations. 2nd ed. Philadelphia: Lippincott-Raven; 1997:1415-1423.
12. Fishman AF. Pulmonary Diseases and Disorders. New York: McGraw-Hill; 1991.
13. Andersen OS. Determination and presentation of acid-base data. Contrib Nephrol. 1980;21:128-136.
14. Carter R. Oxygen and acid-base status: measurment, interpretation, and rationale for oxygen therapy. In: Tiep B, ed. Portable Oxygen Therapy: Including Oxygen Conserving Methodology. Mount Kisco, NY: Futura Publishing; 1991:125-159.
15. Osborne M. Acid-base and fluid-electrolyte abnormalities. Part II: metabolic acidosis. South Med J. 1981;74:1382-1386.
16. Kelman GR, Nunn JF. Nomograms for correction of blood PO2, PCO2, pH and base excess for time and temperature. J Appl Physiol. 1996;21: 1484-90.
17. Gabel RA, Hooper A, Marseglia JJ, Farese G. Calculation and correction of blood gas and acid base variables with a versatile computer program. Anesth Analg. 1981;60:889-896.
18. O’Regan RG, Majcherczyk S. Role of peripheral chemoreceptors and central chemosensitivity in the regulation of respiration and circulation. J Exp Biol. 1982;100:23-40.