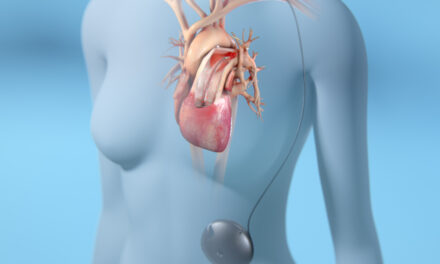
Estrogen was able to reverse the progression of pulmonary hypertension to heart failure and can restore lung and ventricle structure and function in rats, with effects that are maintained even after removal of estrogen, according to researchers at UCLA.
“We were surprised to find this continued benefit, even after we stopped the estrogen treatment,” said the study’s first author, Soban Umar, MD, PhD, a UCLA department of anesthesiology researcher. “These findings suggest that even short-term estrogen therapy may suffice to reverse the disease.”
Using low doses of estrogen, the research team was able to prevent the disease from progressing to right-ventricular heart failure; this did not happen in untreated rats. Systolic blood pressure and ejection fraction also improved, and tests showed that lung weight, which can increase with the disease and result in heart-ventricle enlargement, was also corrected.
Function returned to an almost normal state after 10 days, with nearly full restoration of systolic blood pressure and ejection fraction to normal levels after an additional 12 days. The findings appear in the American Journal of Respiratory and Critical Care Medicine.
Mayo Clinic Joins Global Smoke-Free Worksite Challenge
Mayo Clinic has joined private sector companies, nongovernmental organizations, and governments on a new global campaign to make workplaces around the world smoke-free, according to a recent announcement at the annual Clinton Global Initiative (CGI). The goal of the Global Smoke-Free Worksite Challenge is to expand the number of employees of all sectors able to work in a smoke-free environment.
Partners—including the American Cancer Society, Johnson & Johnson, the Global Business Coalition on Health, and the US Department of Health and Human Services—are committed to making their worksites 100% smoke-free and commit to assist others to do so.
“Mayo Clinic has a leading role, as a larger employer, in creating a smoke-free worksite for close to 30 years,” says John Noseworthy, MD, president and CEO of Mayo Clinic. “We are committed to the needs of our patients and employees, and we are excited to be a partner in this challenge to help make workplaces around the world smoke-free so all employees have the right to clean air.”
The challenge builds on the commitment Mayo Clinic made at the CGI last year. That initiative, called Global Bridges, has worked to build a network of health care providers to lead development of tobacco control and treatment programs in their countries and regions. In less than a year, Global Bridges has trained more than 5,800 health care providers from 31 countries in sessions ranging from short webinars to intensive workshops.
“Secondhand smoke affects everyone,” says Richard Hurt, MD, chairman of Global Bridges and founding director of Mayo’s Nicotine Dependence Center. “This challenge protects workers from secondhand smoke who don’t have any choice. Smokers in a smoke-free environment are more likely to reduce their smoking and increase the chances of them quitting smoking, so it’s healthy for everyone. Right now, over 30 countries across the world have smoke-free workplace laws, which is pretty amazing. We’re hoping to increase that number dramatically with this initiative.
Poractant Alfa Lowers Mortality in Neonatal Respiratory Distress Syndrome Patients
When compared to calfactant (Infasurf), using poractant alfa (Curosurf) in the treatment of neonatal respiratory distress syndrome (RDS) significantly reduced likelihood of death; when compared to beractant (Survanta®), Curosurf produced a “trend toward reduced mortality,” according to results of a study, published in the Journal of Perinatology, comparing all-cause, in-hospital mortality in more than 14,000 preterm infants with the disease. Poractant alfa is marketed as Curosurf by Cornerstone Therapeutics, which holds US licensed rights from Chiesi Farmaceutici SpA (Parma, Italy).
“Cornerstone is extremely pleased with the results of this study. This research, especially among the smallest infants, reinforces why Curosurf is the market leader in the [United States] and worldwide, and why we continue to see successful hospital conversions to Curosurf therapy,” said Craig A. Collard, Cornerstone’s chief executive officer. “When paired with Curosurf’s existing, extensive clinical evidence, we believe these data will give neonatologists further confidence that Curosurf is an appropriate choice to treat babies with RDS.”
Study authors believe the research findings are “critical in neonatal intensive care units (NICUs) as we work to stabilize and improve outcomes in preterm infants who are struggling with RDS.”
Anti-Reflux Surgery Benefits Lung Transplant Patients’ Airway Function
University of Pittsburgh School of Health Sciences researchers have found that surgery to correct gastroesophageal reflux disease (GERD) can preserve lung function in patients with end-stage pulmonary disease both before and after transplantation. Their findings, published in the Archives of Surgery, suggest that esophageal testing should be performed more frequently among these patients to determine if anti-reflux surgery is needed.
GERD is commonly found in patients with end-stage lung disease, particularly those with idiopathic pulmonary fibrosis or cystic fibrosis, and is quite common after lung transplantation. GERD has also been associated with bronchiolotis obliterans syndrome (BOS), a progressive impairment of air flow that is the leading cause of death after lung transplantation.
“It’s possible that reflux, which is due to a weak sphincter between the stomach and esophagus, allows acid and other gastric juices to leak back not only into the esophagus, but also to get aspirated in small amounts into the lungs,” said Blair Jobe, MD, professor of surgery in the cardiothoracic surgery department in the university’s School of Medicine. “That micro-aspiration could be setting the stage for the development of BOS.”
According to Toshitaka Hoppo, MD, PhD, lead author of the study and research assistant professor in the cardiothoracic surgery department, the importance of esophageal testing for reflux in patients with end-stage pulmonary disease is vital. He notes, “Almost one-half of the patients in our series did not have symptoms but were having clinically silent exposure to gastric fluid.” Based on this finding, the research team recommends a very low threshold for esophageal testing in this patient population.
For the study, the researchers reviewed medical charts of 43 end-stage lung-disease patients with documented GERD, 19 of whom were being evaluated for lung transplant and 24 who had already undergone transplantation. All patients were on GERD medications at the time they were evaluated for anti-reflux surgery (ARS), which prevents fluid from leaking back into the esophagus. Prior to ARS, nearly half the patients had either no or mild symptoms of GERD and only a fifth had the typical symptoms of heartburn and regurgitation.
The researchers found that nearly all measures of lung function improved after ARS in both the pre- and post-transplant groups. There also were fewer episodes of acute rejection and pneumonia after ARS in the post-transplant group.
H1N1 More Damaging to Lungs than Seasonal Flu
The 2009 H1N1 pandemic flu virus sets the stage for lethal bacterial infections, according to research in the current issue of mBio®, an open access online journal published by the American Society for Microbiology.
In a mouse study, rodents infected with the virus and Streptococcus pneumoniae had an inflammatory response similar to that in the other mice, but they lacked responses that would repair and regenerate their damaged epithelial cells.
Researchers found that all the mice co-infected with both the 2009 pandemic flu and S. pneumoniae showed severe weight loss and 100% mortality. The lung tissues of the dead mice revealed that the alveoli were severely inflamed and the surfaces of the bronchioles were wiped clean of the protective layer of cells called the epithelium. There was also increased bacterial replication in the lungs of the co-infected mice, a sign that the bacteria were thriving there.
Mice in the study infected with seasonal influenza and S. pneumoniae had slightly enhanced lung tissue damage, but they all survived the dual infections.