Interstitial lung diseases (ILDs) comprise a spectrum of related disorders and correctly diagnosing and treating this diverse group is a challenge to clinicians.
by Paul Nuccio, RRT, FAARC
Interstitial lung diseases (ILDs), frequently referred to as diffuse parenchymal lung diseases, are a heterogeneous, diverse group of pulmonary disorders. These disorders are typically classified together because of the presence of similar clinical, physiologic, pathologic, and roentgenographic manifestations. Environmental and occupational exposures to organic and inorganic dusts, along with other inhaled agents, are the most common causes of ILDs that have been identified. Table 1 shows a classification scheme based on disease etiology. Table 2 lists medications associated with the development of ILD.
The most common symptomatic complaint voiced by ILD patients is progressive dyspnea. This usually begins with exercise and over time progresses to dyspnea at rest. Cough and fatigue are also common complaints. Most patients have abnormalities noted on chest radiographs, although approximately 10% of patients with ILD will present with dyspnea and a normal chest radiograph. Office spirometry testing typically shows abnormalities in lung function.4There are approximately 100,000 hospital admissions related to ILD. According to a study performed in New Mexico, the incidence of ILD in the United States involves 31.5 out of every 100,000 men and 26.1 out of every 100,000 women, with approximately 45% of these individuals having pulmonary fibrosis.1 The incidence of ILD increases with age and with certain disease entities. Physiologic or radiographic evidence of ILD is found in approximately 33% of patients who have rheumatoid arthritis2 and in nearly 100% of those with scleroderma.3 As newer and more sophisticated methods of identifying these disorders are developed, the prevalence of ILD will likely increase.
The clinical assessment of a patient suspected of having ILD involves a thorough history and physical examination, chest radiograph, arterial blood gas (ABG) analysis, lung function testing (PFTs), and routine blood tests. High-resolution computed tomography (HRCT) and bronchoscopy with bronchoalveolar lavage (BAL) also may be helpful.5
Because many ILDs originate as a result of occupational exposures, taking a very detailed, chronological work history is important. Asking questions specific to job responsibilities, types of exposure to chemicals, dusts, and gases, as well as the extent of exposure is vital. The use of any protective equipment also should be discussed.6 Patients should provide as much detail as possible regarding their lifelong occupational and environmental exposure history, since the latency period between exposure and symptoms can be quite lengthy. This information is often obtained through the use of written surveys or questionnaires.
Obtaining a drug history can provide important information to aid in diagnosis. Drug and treatment-induced ILD is quite prevalent. Some patients receiving treatment with bleomycin and other lung cytotoxic drugs who also receive high concentrations of oxygen therapy can develop ILD with diffuse alveolar damage.7
There is a relationship between smoking and the development of ILD, therefore a smoking history must be included in the evaluation. More than 90% of patients who develop eosinophilic granuloma are found to be active smokers at the time the diagnosis is made.8 Genetic factors also can play a role in the development of ILD, so a detailed family history should be documented as well.9
The most common symptomatic complaint expressed by patients with ILD is exercise-limiting dyspnea and, in many cases, an annoying nonproductive cough and fatigue. Although most patients have an accompanying abnormal chest radiograph, approximately 10% of patients presenting with a complaint of dyspnea have a normal chest film.4 Chest pain is uncommon in patients with ILD, but it may be present in cases of ILD associated with systemic lupus erythematosus, rheumatoid arthritis, and some of the drug-induced disorders. Substernal chest pain is common in patients with sarcoidosis.10 Hemoptysis and wheezing are uncommon symptoms with most ILDs, although wheezing can be seen with hypersensitivity pneumonitis or chronic eosinophilic pneumonia. Hemoptysis might be observed with a diffuse alveolar hemorrhage syndrome or lymphangioleiomyomatosis.11
On physical assessment, most patients with ILD are found to have bilateral inspiratory crackles on auscultation. These are generally most prominent in the bases of the lungs. Expiratory wheezes are relatively uncommon. Resting tachypnea and tachycardia also can be present. Late in the disease course, digital clubbing and edema of the lower extremities and/or distension of the jugular veins can be present. Signs of active joint inflammation, joint deformities, and muscular weakness also might be noted.12
Chest radiographs generally, but not always, reveal bilateral reticular or reticulonodular opacities with decreased lung volumes (see Figure 1). In this film, the reticular opacities are most prominent in the right lower lobe. The left lower lobe consolidation in this film obscures the reticular change.
A prone CT image (see Figure 2) shows that the left lower lobe consolidative appearance is due to dense honeycombing. Note the diffuse, somewhat thick-walled, regular cysts of 2-5 mm size. This small size makes the cysts difficult to see on the radiograph. The asymmetry of disease (worse on left) accounts for the greater volume loss in the left lung.
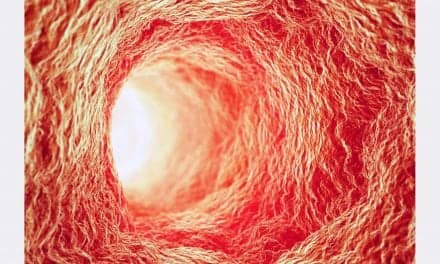
HRCT can be valuable in detecting ILD. It can provide better definition of the location and extent of the disease process as well as the pattern of the disease, due to its improved resolution over a standard chest radiograph. HRCT provides a clearer picture of honeycombing, when present, than does a conventional radiograph.13,14 Because of the greater accuracy in diagnosing ILD with HRCT versus conventional chest radiography, the need for surgical lung biopsy is diminished.
Bronchoalveolar lavage is not considered to be a standard diagnostic procedure in patients with ILD, but it can be an important tool for ruling out infection and helping to establish a diagnosis of hypersensitivity pneumonia. The procedure, wherein a minimum of 100 mL of lavage fluid is instilled into the lungs, can be used to collect cells, inhaled particles, infectious organisms, and solutes from the lower respiratory tract, including the alveolar spaces of the lung.15
Although it is not always possible to make a definitive diagnosis of ILD without an examination of actual lung tissue samples, lung biopsy is not necessary in all patients who are under the suspicion of having ILD. Biopsy can prove to be helpful in assessing disease activity, excluding certain processes that sometimes mimic interstitial diseases, and establishing a definitive diagnosis. It also may be used to help to better predict a patient’s prognosis and potential course of treatment. A biopsy can be performed as part of the BAL procedure or performed as a video-assisted thoracoscopic lung biopsy. which is sometimes the preferred method, particularly for obtaining multiple samples.16
PFTs, including spirometry, lung volumes, and diffusing capacity, are necessary in determining the severity of the illness. Distinguishing between an obstructive and restrictive pattern is beneficial in narrowing down the possible diagnoses. Arterial blood gas samples performed with a patient on room air also should be performed. Most patients with ILD present with a restrictive pattern, with reduced total lung capacity, functional residual capacity, and residual volume. A reduced diffusing capacity is frequently found in ILD patients but is considered a nonspecific finding.17
ILDs, regardless of their etiologies, will progress, and as treatments are developed, the most benefit will be gained if begun early. There is currently no effective therapy for some of the idiopathic interstitial pneumonias (IIPs), such as usual interstitial pneumonia and acute interstitial pneumonia.
Although treatment with corticosteroids is usually recommended for idiopathic pulmonary fibrosis (IPF), this therapy has failed to alter the outcomes in most patients.18 The reason that corticosteroids are still recommended despite the lack of evidence is that no other proven treatment is available, and this therapy has been shown to be effective in treating some of the ILDs. Disorders such as hypersensitivity pneumonia, organizing pneumonia, eosinophilic pneumonia, and desquamative interstitial pneumonia are responsive to corticosteroid treatment. In some patients with IPF or IIP that is progressing slowly, there is suspicion that treatment with corticosteroids or immunosuppressives might contribute to a longer than expected survival.19 IPF generally leads to death within 5 years in approximately 80% of the patients with the diagnosis.
For patients who receive treatment and still experience progressive physiologic deterioration, single lung transplantation should be considered if established criteria are met and no contraindications to the procedure exist. Because the availability of donors is limited, patients who are being considered for lung transplantation should be listed early. It could take up to 2 years before a suitable donor is available.20
Paul Nuccio, RRT, FAARC, is director of respiratory care, Brigham and Women’s Hospital, Boston. For more information, contact [email protected].
References
1. Coultas DB, Zumault RE, Black W, Sobonya RE. The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med. 1994; 150:967-72.
2. Popper MS, Bogdonoff ML, Hughes RL. Interstitial rheumatoid lung disease: a reassessment and review of the literature. Chest. 1977; 62:243-9.
3. Greenwald GI, Tashkin DP, Gong H, et al. Longitudinal changes in lung function and respiratory symptoms in progressive systemic sclerosis. Am J Med. 1987; 83:83-92.
4. Epler GR, McCloud TC, Gaensler EA, Mikus JP, Carrington CB. Normal chest roentgenograms in chronic diffuse interstitial lung disease. N Engl J Med. 1978; 298:934-9.
5. King TE. Approach to the adult with interstitial lung disease. Available at: www.UpToDate.com 2005. Accessed October 15, 2006.
6. Glazer CS, Newman LS. Occupational interstitial lung disease. Clin Chest Med. 2004; 25:467.
7. Cooper JA Jr, White DA, Matthay RA. Drug induced pulmonary disease. Part 1. Cytotoxic drugs. Am Rev Respir Dis. 1986; 133: 321-40.
8. Schwarz ML, King TE. Interstitial Lung Disease. 4th ed. London: BC Decker Inc; 2003.
9. Raghu G. Genetic susceptibility to pulmonary fibrosis. Pulm Perspec. 1995; 12:5-8.
10. James DG. Sarcoidosis of the respiratory system. Semin Respir Med. 1986; 8: 1-111.
11. Schwarz ML, Cherniack RM, King TE. Diffuse alveolar hemorrhage and other rare infiltrative disorders. In: Respiratory Medicine. 2nd ed. Philadelphia: WB Saunders; 1994:1889-1912.
12. Epler GR, Carrington CB, Gaensler EA. Crackles (rales) in the interstitial pulmonary diseases. Chest. 1978; 73:333-9.
13. Muller NL, Miller RR. Computed tomography of chronic diffuse lung disease. Part 1. Am Rev Respir Dis. 1990;142:1206-15.
14. Muller NL, Miller RR. Computed tomography of chronic diffuse lung disease. Part 2. Am Rev Respir Dis. 1990;142:1440-8.
15. Reynolds HY. Use of bronchoalveolar lavage in humans—past necessity and future imperative. Lung. 2000; 178:271-93.
16. Flint A, Martinez FJ, Young ML, Whyte RL, Toews GB, Lynch JP 3rd. Influence of sample number and biopsy site on the histologic diagnosis of diffuse lung disease. Ann Thorac Surg. 1995; 60:1605.
17. Hetta A, Marangio E, Olivieri D. Pulmonary function testing in interstitial lung diseases. Respiration. 2004;71:209.
18. International Consensus Statement. Idiopathic pulmonary fibrosis: diagnosis and treatment. Am J Respir Crit Care Med. 2000; 161:646-64.
19. King TE, Tooze JA, Schwarz MI, et al. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 2001;164:1171-81.
20. Ideopathic pulmonary fibrosis: diagnosis and treatment. International Consensus Statement. Available at: www.thoracic.org/sections/publications/statements/pages/respiratory-disease/idiopathic-19.html. Accessed November 6, 2006.