New data from PTC Therapeutics Inc supports the potential benefit of ataluren in preserving lung function in non-ambulatory nonsense mutation Duchenne muscular dystrophy patients (nmDMD). The results, which are being presented today as part of a company-sponsored symposium, are based on PTC’s analyses of lung function data from one of PTC’s ongoing open-label extension studies (Study 019) versus natural history data from a comparable non-ambulatory cohort.
“We are excited to share the first results available from our long-term DMD extension study in non-ambulatory patients,” said Stuart W. Peltz, PhD, Chief Executive Officer of PTC Therapeutics. “The potential for a therapy to slow disease progression and to improve outcomes beyond ambulation is significant for patients with nonsense mutation DMD.”
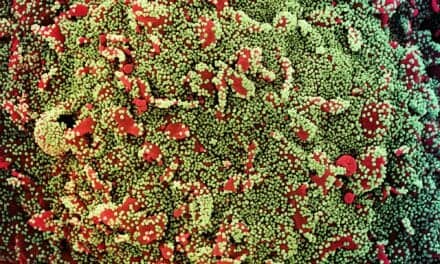
DMD patients experience progressive dysfunction of respiratory muscles, in particular the diaphragm, leading to respiratory failure which is the primary cause of death. Pulmonary function in DMD patients has historically been assessed using forced vital capacity (FVC), a measure of lung function that correlates with disease progression and mortality. FVC tends to peak at an earlier age in DMD patients and then decline more rapidly than in healthy individuals.
The analysis of ataluren’s impact on preservation of lung function is based on FVC, a marker of respiratory insufficiency which progresses with age. The results presented are from a preliminary assessment of pulmonary function in non-ambulatory patients in Study 019 (n = 53). The data were compared with an external control group of patients not receiving ataluren (“untreated”) in a long-term DMD natural history study performed by the Cooperative International Neuromuscular Research Group (CINRG) (n = 114). The CINRG cohort was matched using the following criteria: non-ambulatory (requiring wheelchair use), ? 25 years old, with ? 24 months of corticosteroid use. To reflect the standard of care available during Study 019, only CINRG data from 2012 onward were included.
In order to apply a linear regression model to the analysis, FVC data were log-transformed to achieve a normal distribution. A piecewise linear regression model, which accounts for peak lung function, was utilized. In the untreated natural history cohort, FVC peaked at a mean age of 12.5 years and then declined thereafter. In comparison, ataluren-treated patients achieved peak FVC at a mean age of 16.5 years, a difference of 4 years over the untreated patients. In addition, absolute FVC was 13.8% higher in ataluren-treated patients compared with untreated patients (nominal p = 0.005), which suggests a slower progression of loss in lung function in ataluren-treated patients.
These historically controlled, matched analyses provide insight into the potential pulmonary benefits realized by non-ambulatory ataluren-treated patients versus untreated DMD patients.
“The potential benefit of ataluren in preservation of lung function highlights the long-term benefits of a protein restoration treatment,” stated Professor Francesco Muntoni, MD, Director of the Dubowitz Neuromuscular Centre, University College, London and Great Ormond Street Hospital. “Preserving respiratory function for patients with Duchenne muscular dystrophy is critical.”










My three grandsons all need atralurun they are 4,6,8 years old when will it be approved