With the novel coronavirus able to survive in an aerosolized state for hours, respiratory therapists conducting nebulizer treatments are at increased risk of contracting SARS-CoV-2.
By Lisa Spear
Aerosol therapy is a mainstay treatment for patients with pulmonary diseases, but during the COVID-19 pandemic healthcare workers and caregivers have wondered if delivering aerosolized medications or performing aerosol-generating procedures could spread the novel coronavirus.
While some experts say that the evidence linking aerosol-generating procedures to spread of viral infections is limited by a low amount of research on the topic, clinicians continue to worry that fugitive emission from aerosol therapies could escape into the environment and infect hospital staff and other patients.
“I think a lot more needs to be done to study delivering aerosols to patients who are infected,” said Patricia Dailey, RRT, senior medical science liaison at Aerogen, a company that manufactures aerosol drug delivery supplies.
It’s known that bioaerosols, the aerosols emitted from a cough, carry pathogens, but less is known about how viruses are transmitted as a result of administering medical aerosols that provide essential treatment to pulmonary patients, says aerosol medicine expert Arzu Ari, PhD, RTT, PT, a professor in the Department of Respiratory Therapy at Texas State University.
This has become a particular concern since research published in the New England Journal of Medicine has demonstrated that the novel coronavirus can live for at least three hours suspended in the air.1
Many clinicians have reconsidered the use of nebulizers for their patients during the pandemic, said Ari. Since the number of coronavirus cases started to surge in the United States, she has received a number of emails from clinicians who sought advice on how to effectively treat their patients, while staying safe.
“They are mainly concerned about aerosol drug delivery that they are giving to patients with COVID-19,” she said. “Respiratory therapists didn’t know whether they should deliver aerosolized medications at the hospital. Most of them actually did not want to do any aerosol treatment at the beginning of the pandemic because there were no guidelines. Nobody knew what to do or how to deliver aerosolized medication to this patient population safely and effectively.”
As clinicians become more familiar with treating COVID-19 patients, new guidelines have emerged and experts have come forward to explain how RTs can navigate patient care in a post-COVID world.
According to a new paper published in Respiratory Medicine, Ari writes that with patients with mild COVID-19 cases, clinicians should consider using pressurized metered-dose inhalers (pMDIs) and dry powder inhalers (DPIs) for aerosol drug delivery instead of nebulizers. For this, patients must be awake and able to perform specific breathing techniques with inhalers. It is also essential to use a valved-holding chamber with pMDIs during treatment, the paper says.2
Hospitals are already coping with the coronavirus by using metered dose inhalers to deliver medications instead of using nebulizers, said Cheryl Nickerson, an RT and respiratory product manager with Philips.
Additionally, “when they use nebulizers they are switching to breath-actuated nebulizers that only deliver drug on inspiration or using filters on the expiratory port to mitigate aerosol into the environment,” said Nickerson.
In cases when nebulizers must be used for acute respiratory failure patients, careful consideration should be given to the selection of the device interface since it can impact aerosol emissions.
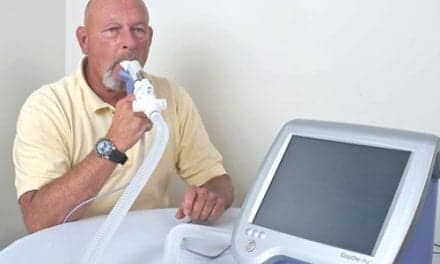
Since nebulizers with facemasks may lead to higher fugitive aerosol emissions, facemasks should be avoided when treating COVID-19 patients.2 Previous research has demonstrated that if a jet nebulizer is used with a facemask, the airflow will force aerosol out of the device during expiration.3 Ari suggests that it’s best to use a mouthpiece with jet and mesh nebulizers.
Conventional jet nebulizers are often used to deliver aerosol therapies, but they may spew two-thirds of the emitted aerosol into the air. These aerosols can potentially expose healthcare providers to both the inhaled medications and the droplets from the patient’s airways, according to the Respiratory Medicine paper. Ari also suggested that using high-efficiency particulate air (HEPA) filters with nebulizers might minimize risk during aerosol drug delivery to patients with COVID-19.
Recently, companies that manufacture jet nebulizers provided filters to use with their devices to use with COVID-19 patients. While the placement of a filter on the nebulizer was effective in capturing exhaled aerosol droplets and reduced second hand exposure of aerosol medication to clinicians, Ari explains that the efficiency of these filters in specifically preventing the transmission of the coronavirus is not completely understood.
Lisa Cambridge, MSHS, RT, director of medical science and pharmaceutical Alliances at PRE Holdings, advises that clinicians should continue to exercise caution and follow guidelines from the US Centers for Disease Control and Prevention. She says always use personal protective equipment (PPE) including N95 masks, when treating patients with COVID-19.4
If possible, maintain six feet of distance from infected patients, especially when a person is coughing or sneezing. When possible, providers should consider using telehealth to evaluate potential coronavirus infected patients to minimize their exposure at healthcare facilities, according to Ari’s paper. For some patients, placing a surgical mask on the patient’s face, especially during coughing, sneezing, or talking, may reduce the risk of viral transmission.
RT
Lisa Spear is associate editor of RT. For more information, contact [email protected].
References
- van Doremalen N, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. NEJM. 2020. doi: https://doi.org/10.1056/nejmc2004973.
- Ari A. Practical strategies for a safe and effective delivery of aerosolized medications to patients with COVID-19, Respiratory Medicine (2020), doi: https://doi.org/10.1016/j.rmed.2020.105987.
- McGrath J, et al. Investigation of fugitive aerosols released into the environment during high-flow therapy. Pharmaceutics, 11 (2019), p. 254
- Centers for Disease Control and Prevention. Interim US guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease. Retrieved on 7/9/20 from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html#table1.