A systematic and step-wise process based upon pH shift is the key to correct interpretation and application of arterial blood gas results.
By Larry H. Conway, BS, RRT, LRCP, FAARC
Published: June 6, 2013
In a previous article, “The Pitfalls of Arterial Blood Gases” (RT, April 2013), I described how simple pre-analytical, analytical, and post-analytical errors can produce arterial blood gas test results (ABGs) that are of little or no value, and perhaps even dangerous. In this article, I will assume that we have avoided all of those pitfalls and and will discuss how to interpret valid ABG results. (Some of the foundational information in this article is necessary for those new to interpreting. I encourage more experienced practitioners to bear with me.)
This article will not attempt to discuss all of the possible causes or disease states that could relate to the results. Neither will it attempt to go into the interpretation of electrolytes or co-oximetry results. Adequate review of these subjects could require—in fact, have required—whole textbooks, and are beyond the scope of this article.

What Is Normal?
To interpret ABGs, we first need to know the normal values for the various analytes. Where do these normal values come from? They mostly come from collected results of volunteers or study subjects who appear to have uncompromised lungs and gas exchange. Researchers plotted the results of the various parameters, found the collective center of the bell-shaped curve of data, and declared the results shown in Table 1.
Table 1. Normal ABG Values
| Analyte | Normal Value | Normal Range* |
| pH | 7.40 | 7.35 to 7.45 |
| PaCO2 (mmHg) | 40 | 35 to 45 |
| HCO3- (mmol/L) | 24 | 21 to 28 |
| PaO2 (mmHg) | 100 | 80 to 100 |
Whichever range you and your facility prefer, it is important to think in terms of a normal range, not a single, specific, always “normal” value—except when it comes to pH for interpreting acid-base balance. We will get to why shortly.
It is also vital to remember that the aggregate “normal” value is a convenient tool, but true normal may be quite different for each individual. Most COPD patients do not have normal ABGs at rest, but their values are normal for them, and are the values we must target when trying to get them through an exacerbation and back to independent living. Most of us who have worked in respiratory care for more than a year have seen this fact overlooked on occasion when efforts are made to wean a COPD patient from a ventilator and have experienced the resulting failures and frustrations.
Oh My, the Physiology!
The relationship of pH, PaCO2 (H2CO3), and HCO3– (and other buffering systems) in the human body is defined by the Henderson-Hasselbach equation:

H2CO3 is carbonic acid and is directly related to and calculable from the PaCO2 (H2CO3 = PaCO2 x 0.3). Thus, H2CO3 represents the contribution of the lungs, while HCO3– represents the contribution of the kidneys in buffering the blood pH. The constant pK, which varies with temperature, is 6.1 at body temperature. So, through simple math and substitution, we get the following equation:

The result is that familiar 7.40 “normal” value that we all know and love.
It’s All About the Relationships
Because in most acute situations the kidneys can only slowly change the HCO3– (24–48 hours), it is essentially unchanging. It is a slow buffer. The PaCO2 can be changed rapidly and is a fast buffer.
The relationship of pH and PaCO2 can be represented as a simple see-saw. When the PaCO2 moves, the pH must move in the opposite direction, since the fulcrum (HCO3-) cannot move quickly.
Figure 1. The pH and PaCO2 have an inverse relationship.

Figure 2. If the PaCO2 falls, the pH rises.

Figure 3. Conversely, if the PaCO2 rises, the pH falls.

The reason for this relationship is the hydration reaction, a rapid and reversible reaction mediated by carbonic anhydrase. The PaCO2 affects the pH very quickly by freeing or trapping free hydrogen ions.

While PaCO2 is not the same thing as CO2 content, the two are directly related. A higher PaCO2 equals a higher CO2 content. If available CO2 rises, the reaction moves left-to-right, releasing free hydrogen ions (H+); the higher the concentration of free hydrogen ions, the more acidic the blood becomes (pH falls). Thus, if a COPD patient in exacerbation begins to retain CO2, the higher level of CO2 pushes the hydration reaction to the right, increasing free H+ concentration and decreasing the pH.
If available CO2 falls, the reaction reverses and removes free hydrogen ions; the lower the concentration of H+, the more alkaline the blood becomes (pH rises). If a patient is breathing rapidly or deeply for any reason, the reaction moves toward the left, decreasing the free H+ concentration and raising the pH.
As I wrote previously, the holy grail of the body is the pH, because it must be maintained in a very narrow range to preserve life. The body will therefore use any tool available to bring pH back toward normal as quickly as possible. The quickest are the lungs and the PaCO2.
Let’s take as an example a diabetic patient in severe diabetic ketoacidosis (DKA), whose available HCO3– is being gobbled up by the acids released by the DKA and is therefore severely acidotic. The body immediately pushes the chest and lungs to blow off CO2 (?) in an attempt to raise the pH as in Figure 2, producing classic Kussmaul breathing. Of course, the body only has the energy to do this for a limited time. If the metabolic cause of the DKA is not resolved or corrected before the energy reserves are depleted, the patient will enter respiratory failure. Respirations will no longer be adequate to correct the acidosis, and the pH will fall rapidly, leading to death.
The relationship of the pH and the HCO3– can be illustrated as a simple lever with one end (PaCO2) unmoving. As shown in Figures 4–6, the fulcrum of the see-saw in Figures 1–3 is now moved from the middle to the end of the lever and from the HCO3– to the PaCO2. Since the PaCO2 can change quickly unlike the HCO3-, this pattern may appear more transiently.
Figure 4. The pH and HCO3– have a direct relationship.

Figure 5. If the HCO3– rises, it will “push” the pH up.

Figure 6. If the HCO3– falls, it will “pull” the pH down.

In the real world, the relationships shown in Figures 5 and 6 can take place simultaneously. As the HCO3– changes, for whatever reason, the pH changes. The body’s mechanisms for homeostasis push the lungs to react and change the PaCO2 in a way to mitigate the pH change (Figures 2 and 3). Both relationships are constantly at work, balancing and complementing each other, one fast and one slow, until one or the other goes out of control, is overwhelmed by an external factor, or is unable to act.
A Word or Two About Oxygenation
When it comes to interpreting ABGs, everyone sweats the acid-base, and oxygenation can become an afterthought. It should not. While pH has a very narrow range of safety, hypoxia can be just as deadly and damaging, as many of us have observed.
As with any diagnostic test, it is incumbent upon clinicians to assess the accuracy and value of a result. They must ask, “Is this reported PaO2 believable or relevant given the environment in which the sample was obtained?” This can be assessed in numerous ways, including the use of the alveolar gas equation…
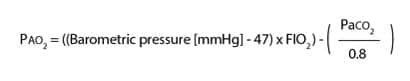
…and correlation to the patient’s clinical status. Numerous reasons the value might be incorrect were discussed in my previous article. If the reported PaO2 is higher than physiologically possible from the above equation, it must be doubted and rechecked.
There are some special considerations about oxygenation that can make it seem less precise than acid-base, and that may be one of the reasons it is not as sharply focused upon as acid-base. One such consideration is that, unlike pH and PaCO2, there is an expected and predictable reduction of PaO2 based upon age. Therefore, what is considered normal PaO2 declines with age. This decline is defined in a variety of ways but the following are two common rules-of-thumb:
- normal PaO2 decreases 1 mmHg for every year over age 60
- PaO2 ? 110 – (age x 0.5)
Hypoxemia is categorized as mild, moderate, or severe, based upon the divergence from the normal range. Like most medical normal values and ranges, the definition can vary slightly, but generally the following definitions apply:
- Mild hypoxemia: PaO2 = 60 to 79 mmHg
- Moderate hypoxemia: PaO2 = 40 to 59 mmHg
- Severe hypoxemia: PaO2 < 40 mmHg
A point of contention regarding oxygenation is the application of the term normal relative to oxygenation. A PaO2 that is within normal range while the patient is on supplemental oxygen is not necessarily normal. For example, a PaO2 of 86 mmHg while breathing an FiO2 of 0.8 is not normal; in a patient with no respiratory disorders, the Pao2 on a 0.8 FiO2 should be about 500 mmHg. This PaO2 is in the normal range only by virtue of the supplemental oxygen; it would plummet to crisis levels if the supplemental oxygen were removed. Given the minimal change of PaO2 in the presence of such a high FiO2, this could even be termed refractory hypoxemia. For clarity, it is best termed corrected or partially corrected, but not normal. This will prevent lots of possible subsequent clinical errors for or by members of the health care team.
The alveolar-arterial PO2 gradient (A-a gradient) is helpful in determining just how abnormal the corrected PaO2 value is. It uses the PaO2 from the alveolar gas equation:
A – a gradient = PAO2 – PaO2
It shows how widely the PaO2 varies from the anticipated value for a given FiO2. Considering the example in the previous paragraph, the A-a gradient is 530 – 86, or 444. A quick estimate for the normal A-a gradient can be obtained by dividing the age of the patient by 4 and adding 4 to the result. Even at age 100, the normal A-a gradient is not over 30, so the hypoxemia in this example is highly nonresponsive to FiO2 (refractory).
Interpretation and Clinical Use
With the relationships and factors above firmly in mind, let’s look at some ABG results. As I said previously, for purposes of interpretation we should consider normal pH absolute 7.40. This is so that what I term the primary pH displacement can be clearly identified without confusion or issues of overcompensation. The body does not, on its own, overcompensate. Therefore:
- If the pH is below 7.40, the primary disorder is presumed to be an acidosis.
- If the pH is above 7.40, the primary disorder is presumed to be an alkalosis.
Once these relationships are understood, the interpretation process is straightforward:
- Acidic or alkaline: determine whether the primary pH displacement was acidosis or alkalosis.
- Buffer of blame: determine which buffers (PaCO2 or HCO3-) would cause the primary pH displacement.
- If caused by PaCO2, the disorder is respiratory.
- If caused by HCO3-, the disorder is metabolic.
- If both cause the pH displacement, it is a combined respiratory and metabolic disorder.
- Combine: steps 1 and 2 together define the disorder. For instance, if step 1 indicates acidosis and step 2 indicates a respiratory issue, the disorder is respiratory acidosis.
- Determine if there is any compensation in effect.
- If the non-causative buffer (the one that did not cause the primary pH displacement) would have no impact on the pH displacement, or the pH remains well outside the normal range, the disorder is uncompensated.
- If the non-causative buffer would correct the pH displacement and the pH is approaching the normal range, the disorder is partially compensated.
- If the non-causative buffer would correct the pH displacement and the pH is within the normal range, the disorder is fully compensated.
- Determine whether the PaO2 is believable relative to the alveolar gas equation and patient clinical presentation. If not, reject the result.
- If the PaO2 is within the normal range and the sample was obtained on room air, this is normal oxygenation.
- If it is within normal range but the sample was obtained on supplemental oxygen, this is best called corrected hypoxemia.
- If the value is below the age-adjusted normal range, determine the degree of hypoxemia.
Using the steps above, let us consider several examples and interpret the ABG results.
Example 1. A 55-year-old patient:
pH = 7.25
PaCO2 = 39 mmHg
HCO3– = 16 mmol/L
PaO2 = 94 mmHg
FiO2 = 0.21
Following the steps defined above, we see that:
- The pH (below 7.40) indicates that the primary pH displacement is acidosis.
- A normal PaCO2 would not cause acidosis, but the low HCO3– would. The disorder is therefore metabolic in origin.
- Combining the first two results indicates metabolic acidosis.
- The PaCO2 has not changed (assuming that this patient’s PaCO2 is normally near 40 at rest), and the pH remains well outside the normal range. This is therefore an uncompensated metabolic acidosis.
- The PaO2 is consistent with the alveolar gas equation and the A-a gradient is within normal limits. The PaO2 is within the normal range and the sample was not obtained on supplemental oxygen, so the oxygenation is normal. The diagnosis, therefore, is uncompensated metabolic acidosis with normal oxygenation.
Example 2. A 55-year-old patient:
pH = 7.25
PaCO2 = 75 mmHg
HCO3– = 30 mmol/L
PaO2 = 39 mmHg
FiO2 = 0.21
- Again, the pH is acidotic.
- The HCO3– would not cause acidosis, but the high PaCO2 would. Therefore, the causative buffer is the PaCO2 and the disorder is respiratory.
- Combining these two findings shows that this is a respiratory acidosis. Since the HCO3– is elevated but has not had time to respond to the pH, this is likely an acute disorder imposed on a chronic condition.
- The noncausative buffer (HCO3-) has not changed to correct the pH, and the pH remains well outside the normal range, so this is uncompensated respiratory acidosis.
- The PaO2 is consistent with the alveolar gas equation and the A-a gradient is marginal. This is severe hypoxemia, likely secondary to the elevated PaCO2. In this case, the diagnosis is uncompensated respiratory acidosis with moderate hypoxemia. This could be a COPD patient in acute crisis.
Example 3. A third 55-year-old patient:
pH = 7.36
PaCO2 = 18 mmHg
HCO3– = 14 mmol/L
PaO2 = 110 mmHg
FiO2 = 0.21
- Here, the pH is within normal limits, but acidic (below 7.40).
- The PaCO2 is low, but would not cause the pH to fall below 7.40 (Figure 2). The HCO3– is quite low and would cause the pH to fall (Figure 6). This was initially a metabolic problem.
- Combining the first two results, we determine that this is a metabolic acidosis.
- The PaCO2 has moved in a direction that would correct the pH displacement, and in fact the pH is back in the normal range. This is fully compensated metabolic acidosis. How long it will remain compensated depends on how long the patient can continue to breath to keep the PaCO2 this low, and whether the metabolic component gets worse.
- The PaO2 is unexpectedly high, but possible with the low level of the PaCO2. It is consistent with the alveolar gas equation and the A-a gradient, and is therefore normal. The diagnosis is thus fully compensated metabolic acidosis with normal oxygenation. Many of us have seen patients similar to this. It could easily be a patient with DKA in the ER.
Example 4. A 15-year-old patient:
pH = 7.49
PaCO2 = 18 mmHg
HCO3– = 14 mmol/L
PaO2 = 110 mmHg
FiO2 = 0.21
- The pH is above 7.40, so the primary displacement was alkalosis.
- The low PaCO2 would cause the alkalosis; the low HCO3– would not. Therefore, this is a respiratory disorder.
- Putting these two findings together, we see that this is respiratory alkalosis.
- The HCO3– has had time to lower to correct the pH to near the normal range. This has therefore been going on for at least 24 hours, and is partially compensated.
- The PaO2 is again unexpectedly high but compatible with the alveolar gas equation, and the A-a gradient is normal. No supplemental oxygen is present, so oxygenation is normal. The diagnosis is partially compensated respiratory alkalosis with normal oxygenation. This demonstrates the importance of getting step A correct. This could be a patient who has been struggling with an asthma crisis for several hours, or has some neurological drive to hyperventilate, as opposed to the DKA patient previously described. The only difference was the direction of the primary pH displacement.
Example 5. A 38-year-old patient:
pH = 7.49
PaCO2 = 46 mmHg
HCO3– = 30 mmol/L
PaO2 = 85 mmHg
FiO2 = 0.35
- The pH is displaced to alkalosis.
- The elevated HCO3– explains the alkalosis, so this is a metabolic issue.
- Combining these two findings indicates metabolic alkalosis.
- The PaCO2 elevation would work to correct the pH, but the pH remains just outside the normal range, so this is partially compensated.
- The PaO2 is within the normal range with supplemental oxygen of 35%, and so demonstrates fully corrected hypoxemia. This may have nothing to do with the acid-base disturbance. The resulting diagnosis is partially compensated metabolic alkalosis with fully corrected hypoxemia. This could be a patient with, for example, sarcoidosis causing the hypoxemia, and a chronic abuse of antacids causing the alkalosis. The body will allow the PaCO2 to rise to some degree to correct the metabolic disorder, but, unless sedated, will not generally allow excessive hypoventilation or respiratory cessation for that purpose.
Example 6. A 65-year-old patient:
pH = 7.38
PaCO2 = 65 mmHg
HCO3– = 32 mmol/L
PaO2 = 62 mmHg
FiO2 = 0.21
- The pH is slightly below the absolute normal of 7.40, so it indicates acidosis.
- The PaCO2 is the buffer that would cause the acidosis, so this is a respiratory disorder.
- These combined findings indicate respiratory acidosis.
- The HCO3– has corrected the pH back to within normal range so this is fully compensated.
- There is a mild hypoxemia (PaO2 between 60 and 79 mmHg). The diagnosis is therefore fully compensated respiratory acidosis with mild hypoxemia. This could be the COPD patient from a few examples prior, in their normal non-crisis state.
Don’t Forget X, Y, and Z
There are unlimited possible disturbances and compensations involving these analytes. I hope that the above examples have demonstrated the key factors in ABG interpretation. It is important to remember that an ABG is only a snapshot in time. That snapshot can be totally changed within moments. Without considering the snapshots that came before, a worsening crisis could be mistaken for a resolving one. Further, without a baseline ABG, it is more difficult to know for certain what has happened to the patient, how to correct it most effectively, and what should be the appropriate target for a return to “normal.”
Finally, remember that once we begin intervention with ventilators, BiPAP, oxygen, and other modalities and therapies, many of the assumptions discussed in this article go out the window. While the body generally does not overcompensate, we can and often do (intentionally or unintentionally) overcompensate. We can and do push pH to the other side of normal, through medications or ventilator support. Therefore, caution must be used in determining the cause and effect in acid-base disorders once we introduce our external influences into the mix.
RT
Larry H. Conway, BS, RRT, LRCP, FAARC, is the chief of respiratory service for the VA Medical Center in Washington, DC. For further information, contact [email protected].











Great ABG lesion, I really enjoy working with the sample questions and learning about the diseases associated with each of them.